Trends of red cell alloimmunization in β thalassemia major patients: A single center retrospective study in Karachi
2 Department of Research & Study, AMTF Helping Blood disorder, Karachi, Pakistan, Email: oncomansoor@hotmail.com
3 Department of Pharmacy Services & Education, AMTF Helping Blood disorder, Karachi, Pakistan, Email: anwari@amtf.edu.pk
4 Department of Biostatistics, AMTF Helping Blood disorder, Karachi, Pakistan, Email: humairama@amtf.edu.pk
Received: 06-Dec-2017 Accepted Date: Dec 20, 2017; Published: 05-Jan-2018
Citation: Qidwai A, Mansoor N, Syeda A, et al. Trends of red cell alloimmunization in β thalassemia major patients: A single center retrospective study in Karachi. J Blood Disord Treat. 2018;1(1):3-5.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
OBJECTIVE: To determine the frequency of red cell alloimmunization and identify the common alloantibodies among patients with β Thalassemia major.
METHODS: The records of 372 β Thalassemia major patients on regular blood transfusion at Afzaal Memorial Thalassemia Foundation (AMTF) were reviewed to determine the history of blood transfusion and frequency rate for alloantibodies.
RESULTS: Red cell alloantibodies had an overall ratio of 10.75% (40 patients). Thirty-Two patients (80%) among those had single antibody while eight (20%) had multiple antibodies. The most commonly occurred antibodies were E (32.5%) and K (27.5%). The mean age of patients with alloimmunization was 10.63 years (SD ± 5.587). The splenomegaly was reported in thirty-one (77.5%) and hepatomegaly in eighteen (45%) patients. One patient had splenectomy.
CONCLUSION: The occurance rate (10.75%) of alloimmunization in this study can most likely be explained by thesimilarity in the ethnicity between patients and donors. In this study, higher rate of alloimmunization is observed in patients received first transfusion at an early age, secondary to more number of transfusions. Further studies are required to evaluate the association of splenectomy with alloimmunization. The transfusion of phenotypically matched blood is essential for transfusion dependent patients. Considering the high frequency of anti-E and anti-K, it is advisable to genotype patients and donors for respective antigens in order to avoid alloimmunization.
Keywords
Alloimmunization; Beta thalassemia; Blood transfusion
The thalassemia syndrome is a heterogeneous group of inherited disorders caused by genetic lesions leading to decrease synthesis of one or more of the globin subunit [1]. Thalassemia occurs with high frequency in a broad belt extending from the Mediterranean basin through the Middle East (Iran), India and Southeast Asia [2,3]. Major complications related to frequent blood transfusions in β thalassemia major includes iron overload, multi organ damage and alloimmunization to erythrocyte antigens [1,4-8]. Alloimmunization is a transfusion complication which may occur in immunocompetent transfusion dependent recipients. Blood is matched routinely only with respect to ABO antigens as well as D antigen which is the most important member of the Rh blood group system. Therefore, there is a probability that a donor may have that red cell antigen not present in the recipient, this disparity of blood group system can lead to alloimmunization [4,5,9-12]. The etiology of alloimmunization has multiple origins and comprises primarily of three contributing factors including antigenic variations of red blood cells and differences between donor’s and the recipient’s blood, immune status of the recipient and the immunomodulatory effect of the allogenic blood transfusions on the recipient’s immune system [1,4,5,7,11]. Alloimmunization is a serious and unfortunate complication that causes difficulty in obtaining compatible blood, delayed transfusion reactions and even occasional life-threatening events [5-8,12]. The frequency of alloimmunization to red cell antigens in thalassemia major patients has varied from 5-30% [4,9]. Previous research shows that the late start of blood transfusion and irregular frequency increases the incidence of alloimmunization in β Thalassemia patients [8,11,13]. Early and regular blood transfusion therapy in thalassemia patients decreases the complication of severe anemia and enhances duration of survival [8,11,13]. Alloimmunization is often a less significant problem among patients where transfusion was initiated before the age of 3; however, it has also been reported that alloimmunization is reduced if transfusion is commenced before the age of 5 [5,11,13]. There is a high frequency of alloimmunization in splenectomised beta thalassemia patients reported in literature. The nonfunctional spleen or absence of spleen in patients with beta thalassemia causes augmentation of immune response against transfused foreign antigens [5]. In transfusion dependent thalassemia patient, frequency of red cell autoantibodies is less than the rate of alloimmunization [6-8]. Consequences of auto antibodies include difficulties in finding compatible blood, cross matching and because of more transfusion reactions possibility of life threatening reactions [6-8]. Thalassemia is most common amongst inherited haemoglobin disorders in Pakistan becoming one of the major public health problems [14-16]. The issue is compounded through limited availability of data on the incidence of RBC alloimmunization in transfusion-dependent thalassemia patients in Pakistan. In the present retrospective study we analyze the frequency of alloimmunization in thalassemia patients and evaluation of factors responsible in the occurrence of such complications.
Methods
This single centre retrospective study was conducted at Afzaal Memorial Thalassemia Foundation (AMTF), Karachi Pakistan. A total of 372 β Thalassemia major patients on Hb electrophoresis or HPLC were included to determine the history of blood transfusion and frequency rate for alloantibodies. Patients with other hematological disorder or who did not show compliance to regular treatment protocols or lost to follow-up were excluded. Variables of interest were age, gender, status of spleen and detection of red cell alloantibodies.
Statistical Analysis
Data was analyzed using statistical packages for social science (SPSS). Descriptive statistics frequency and percentage were computed for qualitative observations while mean and standard deviation were estimated for quantitative measurement.
Result
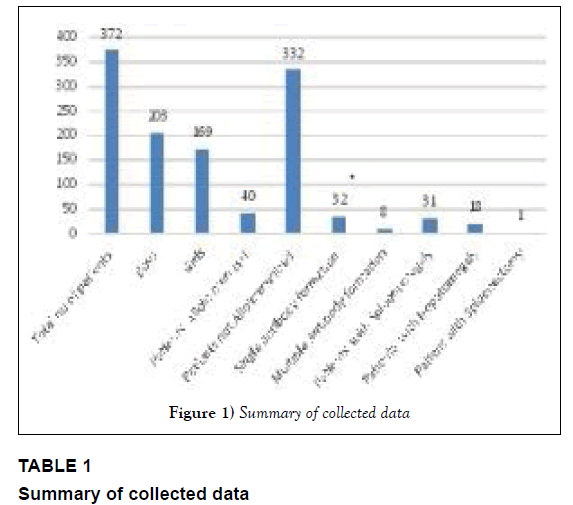
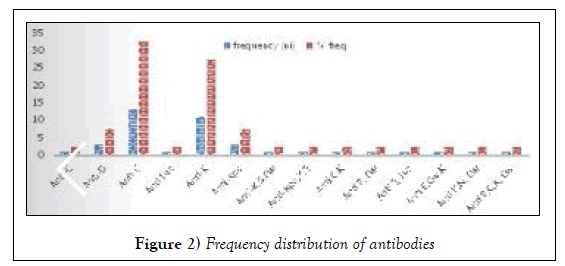
From the total of 372 patients included in this study, 203 (54.56%) patients were male and 169 (45.43%) patients were female. Out of which, 18 males and 22 females were found as positive cases for alloimmunization. Hence, male to female ratio was 1:1.2. 40/372 (10.75%), were identified to have red cell alloantibodies and 332 (89.24%) were negative for alloantibodies. Among 40 positive patients, 32 (80%) had single alloantibodies while 8 (20%) patient had multiple antibodies (Table 1 and Figure 1). The mean age of patients with alloimmunization was 10.63 years (SD ± 5.587). The distribution of alloantibodies was shown in Table 2 and Figure 2, respectively.
| Diagnosis | Beta Thalassemia Major |
|---|---|
| Total no of patients | 372 |
| Boys | 203 |
| Girls | 169 |
| Patients Alloimmunized | 40 |
| Patients not Alloimmunized | 332 |
| Single antibody formation | 32 |
| Multiple Antibody formation | 8 |
| Patients with Spleenomegaly | 31 |
| Patients with Hepatomegaly | 18 |
| Patient with Spleenectomy | 1 |
Table 1: Summary of collected data
| S. No. | Type of Antibody | Frequency (ni) | % freq |
|---|---|---|---|
| 1 | Anti-C | 1 | 2.5 |
| 2 | Anti-D | 3 | 7.5 |
| 3 | Anti-E | 13 | 32.5 |
| 4 | Anti-Lea | 1 | 2.5 |
| 5 | Anti-K | 11 | 27.5 |
| 6 | Anti-Kpa | 3 | 7.5 |
| 7 | Anti-K, S, Cw | 1 | 2.5 |
| 8 | Anti-Kpa, K, E | 1 | 2.5 |
| 9 | Anti C, K | 1 | 2.5 |
| 10 | Anti E, Cw | 1 | 2.5 |
| 11 | Anti E, Jka | 1 | 2.5 |
| 12 | Anti E, Cw, K | 1 | 2.5 |
| 13 | Anti K, N, Cw | 1 | 2.5 |
| 14 | Anti E, C, K, Cw | 1 | 2.5 |
| Total | 40 | 100 |
Table 2: Frequency distribution of antibodies.
The mean age at first transfusion in patients with alloimmunization was 7 months and without alloimmunization it was 13 months. Among the 40 patients from the alloimmunized group splenomegaly was reported in thirty one (77.5%) and hepatomegaly in eighteen (45%) patients, while one patient had splenectomy.
Discussion
This retrospective analysis to identify the frequency and distribution of alloimmunization in beta thalassemia patients showed frequency (10.75%) of alloimmunization which is comparable with various reported literature varied from Pakistan such as 2.8%-6.8% to 7.4%-9.2% and 11.8% [5,6,8,10,11,17-19]. The occurrence of alloimmunization could be related to red cell homogeneity between the donor and recipient population in this region [8,17]. A local study conducted in 2011, showed low frequency of alloimmunization, i.e., 3.75% in transfusion dependent beta thalassemia patients [20]. High occurrence of antibodies (47.7%) against the Rh system had previously been reported in number of studies [5,7,10,13,18,19,21]. Higher rate of alloimmunization has also been reported in Kuwait (22%) south-western neighbor of (Iran 22.8%). The underline factors behind such higher rate of alloimmunization may be due to the heterogeneity of the population, lack of better matched donors for those patients & use of post storage leucodepleted blood [10,22]. Amongst the alloimmunized group all patients had spleen intact and the majority had splenomegaly, while in the non alloimmunized group three patients were reported with splenectomy. Previously published studies showed higher rate of alloimmunization among splenectomised patients than those who did not have splenectomy [22]. In contrast to the published literature, higher incidence of alloimmunization in splenectomised patients due to the development of immune response was not observed in our analysis [5]. However, only one patient had splenectomy therefore further data is required to evaluate the association of splenectomy with alloimmunization. Another previously published study states that differential rate of splenectomy as a risk factor between patients with and without alloimmunization is not statistically significant [11]. Whereas a recent published study reported that splenectomy is strongly associated with increased alloimmunization in beta thalassemia major patients [23]. Blood transfusion for all alloimmunized thalassemia patients started at an early age where the mean age was 7 months; probably the reason is more number of blood transfusions. This is in contrast to other studies which showed low rates of alloimmunization in patients with early onset of transfusion, there is a possibility of some type of immune tolerance towards repeated blood transfusions [4,11,13]. Infants have shown lower incidence of alloimmunization towards blood cell antigen and there are less transfusion reactions reported in infants [11]. It was found in previous studies that rate of alloimmunization is increases with age [24]. The results of our study show that there was no noteworthy association among alloimmunization and gender [8,11]. Of forty patients with alloimmunization, male to female ratio was 1:1.2 with P-value 0.99. Previously published studies also revealed that there is no influence of gender on rate of alloimmunization [24]. However, one study published from Iran showed higher incidence on alloimmunization in male patients [22]. In our study most common detected antibodies are anti-E and anti-K, that is comparable with other studies which reported alloantibodies that were directed against antigens in the Rh and Kell systems [5,7,10,13,18,19,21]. A recent study published from Iran reported 11 out 272 patients developed anti-D [22] however, in our study Anti-D antibody is identified only in 3 patients who were Rh negative, received transfusion of Rh positive blood due to unavailability of Rh negative blood.
It is also known that these blood groups are thought to be strongly immunogenic and most of the studies have shown the alloantibodies against Kell and Rh system [5,7,10,13,18,21]. Other studies in Pakistan have also shown comparable results where RBC alloantibodies belonged mainly to Rh system although other antibodies such as anti-K, anti-Jsb and anti-Jka were also detected [5,7].
Conclusion
Alloimmunization is an important complication related to blood transfusions in beta thalassemia major. Multiple factors may play a contributing role that includes antigenic variations of red blood cells and differences between donor’s and the recipient’s blood, immune status of the recipient and the immunomodulatory effect of the allogenic blood transfusions on the recipient. The exact mechanism and kinetic is not very clear however, low alloimmunization rate in this study can most likely be explained by the similarity in the ethnicity between patients and donors. We conclude that the matter of alloimmunization in thalassemia patients is reasonably significant in both clinical and laboratory practice but the reported literature from Pakistan is very scanty. Alloimmunization should be watched carefully in beta thalassemia patients and should be evaluated in all beta thalassemia patients if they repeatedly suffer from transfusion reaction or unable to maintain hemoglobin at required levels in spite of being regularly blood transfused.
Although preventive measures like haemovigilance are important but more data from large centers will help in finding the results related to red cell alloimmunization in this part of the world. Despite the fact that considerable cost would incur collecting data but resource allocation to address this issue is extremely important.
This study re-emphasize the RBC antigen typing before first transfusion and issue of antigen matched blood, at least for Rh and Kell antigens. Transfusion of phenotypically matched cells for selective antigen may reduce the risk of alloimmunization.
Implementation of molecular genotyping for transfusion has been limited primarily to reference laboratories but it can be adapted to screen donor RBCs. Mass scale genotyping of blood donors would increase the availability of antigen negative RBCs and be used to recruit individuals whose blood type is needed. Performing an extended RBC genotyping on all patients can identify the antigens that put the patient at risk of alloimmunization and potentially improve outcomes if clinically significant antigen negative RBCs are available. The application of genotyping for patients and donors will undoubtedly decrease alloimmunization and improve transfusion therapy, but whether the cost will be prohibitive has yet to be determined.
REFERENCES
- Sadeghian MH, Keramati MR, Badiei Z, et al. Alloimmunization among transfusion-dependent thalassemia patients. Asian J Transfus Sci. 2009;3:95-8.
- Angastiniotis M, Modell B. Global epidemiology of hemoglobin disorders. Ann N Y Acad Sci. 1998;850:251-69.
- Rezaei N, Naderimagham S, Ghasemian A, et al. Burden of hemoglobinopathies (thalassemia, sickle cell disorders and G6PD deficiency) in Iran 1990-2010: Finding from the global burden of the disease study 2010. Arch Iran Med. 2015;18:502-7.
- Singer ST, Wu V, Mignacca R, et al. Alloimmunization and erythrocyte autoimmunization in transfusion-dependent thalassemia patients of predominantly Asian descent. Blood. 2000;96:3369-73.
- Hassan K, Younus M, Ikram N, et al. Red cell alloimmunization in repeatedly transfused thalassemia major patients. Department of Pathology, Pakistan Institute of Medical Sciences, Islamabad. Int J Pathol. 2004;2:16-9.
- Beutler E. rTansfusion medicine: Williams Hematology, ed: 6th chapter;140:1879-88.
- Bilwani F, Nabi G, Adil SN, et al. Frequency of irregular red cell alloantibodies in patients with thalassemia major: A bicenter study. J Pak Med Assoc. 2005;55:563-5.
- Noor MN, Haslina NA. Red cell immunization in multiply transfused Malay thalassemic patients. Southeast Asian J Trop Med Public Health. 2006;37:1015-20.
- Hoppe CC. Newborn screening for non-sickling haemoglobinopathies. Hematology 2009;1:19-25.
- Ameen R, Al-Shemmari S, Al-Humood S, et al. RBC alloimmunization and autoimmunization among transfusion-dependent Arab thalassemia patients. Transfusion. 2003;43:1604-10.
- Shamsian BS, Arzanian MT, Shamshiri AR, et al. Frequency of red cell alloimmunization in patients with ß-major thalassemia in an Iranian Referral Hospital. Iran J Pediatr. 2008;18:149-53.
- Vichinsky EP, Earles A, Johnson RA, et al. Alloimmunization in sickle cell anemia and transfusion of racially unmatched blood. N Engl J Med. 1990;322:1617-21.
- Layla AM, Bashawri MD, Malik SA, et al. Red cell alloimmunization in thalassemia patients. Bahrain Med Bull. 2005;27(2).
- Waheed U, Satti HS, Farooq N, et al. Frequency of haemoglobinopathies: A single-centre, cross-sectional study from Islamabad, Pakistan. East Mediterr Health J. 2012;18:1257-9.
- Ahmed S, Petrou M, Saleem M. Molecular genetics of beta-thalassaemia in Pakistan: A basis for prenatal diagnosis. Br J Haematol. 1996; 94:476-82.
- Ansari SH, Shamsi TS, Ashraf M, et al. Molecular epidemiology of ß-thalassemia in Pakistan: Far reaching implications. Indian J Hum Genet. 2012;18:193-7.
- Ho HK, Ha SY, Lam CK, et al. Alloimmunization in Hong Kong southern Chinese transfusion-dependent thalassemia patients. Blood. 2001;97(12):3999-4000.
- Sadeghian MH, Keramati MR, Badiei Z, et al. Alloimmunization among transfusion-dependent thalassemia patients. Asian J Transfus Sci. 2009;3:95-8.
- Bhatti FA, Salamat N, Nadeem A, et al. Red cell immunization in beta thalassaemia major. J Coll Physicians Surg Pak. 2004;14:657-60.
- Muhammad U, Moin S, Moinuddin M, et al. Frequency of red cell alloimmunization among patients with transfusion dependent beta thalassemia. Pak Int J Hematol Oncol. 2011;21:166-9.
- Ansari S, Voosogh P, Moshtaghian S. Assessment of frequency of alloimmunization and erythrocyte autoimmunization in transfusion dependent thalassemia patients. Acta Medica Iranica. 2008;46:137-40.
- Hussein E, Desooky N, Rihan A, et al. Predictors of red cell alloimmunization in multitransfused Egyptian patients with ß-thalassemia. Arch Pathol Lab Med. 2014;138:684-88.
- Junsuwan S, Tangvarasittichai O, Tangvarasittichai S. Alloimmunization to red cells and the association of alloantibodies formation with splenectomy among transfusion dependent ß-thalassemia major/Hb E patients. Ind J Clin Biochem. 2015;30:198-203.
- Datta SS, Mukherjee S, Talukder B, et al. Frequency of red cell alloimmunization and autoimmunization in thalassemia patients: A report from eastern India. Adv Hematol. 2015;610931.