Two cystoceles that hide different pathophysiological histories: Report of two cases
2 Department of Urology, University Hospital Ibn Sina, University Mohammed V, Rabat, Morocco
Received: 08-Nov-2018 Accepted Date: Nov 24, 2018; Published: 30-Nov-2018
Citation: Slaoui A, Nah A, Bargach S, et al. Two cystoceles that hide different pathophysiological histories: Report of two cases. Surg Case Rep. 2018;2(2):37-38.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
BACKGROUND: The most commonly affected compartment in pelvic organ prolapse is cystocele. For a long time, vaginal birth was considered being the most important factor when it comes to its primary occurrence. However, recent studies showed that non-obstetric risk factors should also be considered.
CASE PRESENTATION: In our study, we report the cases of two women having advanced cystocele but with different medical history. The first one was a 49-year-old white woman G7P5 all vaginally without any other medical history and with a BMI of 25.7. She was treated successfully using a laparoscopic approach to suspend the bladder to the sacral promontory. The second one was a 70-year-old widow G0P0 followed for type II diabetes under insulin therapy with a BMI of 31.6. She benefited from a colpocleisis. Both women were controlled 4 weeks later and annually and didn’t demonstrate any complication or recurrence.
CONCLUSION: Despite the fact that both patients presented the same pathology, their pathophysiological records were significantly different. Through this work we hope to inform the general public about this pathology that can cause important functional disorders in women’s bodies and could in some cases be the cause of a social discomfort and tensions within the couple. Finally, it is essential to highlight that non-obstetric risk factors that can be modified or controlled can provide an effective primary prevention ground.
Keywords
Cystocele; Pelvic organ prolapse; Vaginal delivery; Risk factors
Introduction
Cystocele is described by a hernia of the posterior side of the bladder that pushes back and forth the anterior side of the vagina [1]. For a long time, vaginal birth was considered being the most important factor when it comes to the occurrence of primary POP; however, recent studies showed that non-obstetric risk factors should also be considered [2]. Due to a real taboo surrounding this disease in Morocco, the number of affected patients remains underestimated. We report two cases of women with advanced cystocele, which required a surgical procedure to avoid further complications. By careful analysis of the two patient’s profile and comparing them to the data from the literature, we will try to understand the pathophysiology of this disease in order to better treat or even prevent it.
Case Presentation
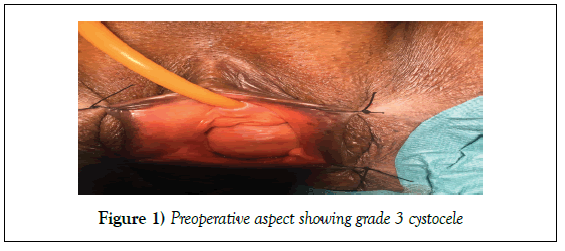
First, we report the case of a 49-year-old white woman G7P5 all vaginally without any other medical records and with a body mass index of 25.7. The patient had dyspareunia and vaginal mass sensation. Clinical examination revealed a grade III cystocele (Figure 1). The prolapse was treated successfully using a laparoscopic approach to suspend the bladder to the sacral promontory (laparoscopic promontofixation). She was controlled 4 weeks later and annually and didn’t demonstrate any complication or recurrence.
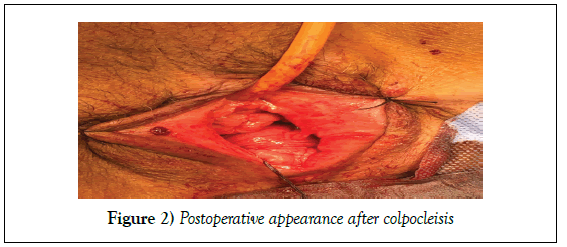
The second case is a 70-year-old widow G0P0 followed for type 2 diabetes under insulin therapy with a body mass index of 31.6, she was initially presented for repeated urinary tract infections, urinating gene and chronic feeling of perineal heaviness. The valve clinical examination revealed grade III cystocele. Since the patient was widowed and unwilling to have sexual activities, we opted for colpocleisis (Figure 2).
She was controlled 4 weeks later and annually and didn’t demonstrate any complication or recurrence.
Discussion
Life expectancy significantly increased those last decades. The aging of body tissues makes them weaker, which can lead to an upsurge of certain pathologies such as cystocele. Morocco being a conservative country, sex is taboo and some sexual questions remain unsolved. As a result, Moroccan patients avoid medical examinations due to the social pressure and their low self-esteem. When there is dyspareunia, patients consult a doctor mostly to avoid divorce. In this article, we propose to review the literature, in order to better understand the pathophysiology of the cystocele and raise awareness about this pathology that remains unknown from the public. Numerous epidemiological studies have focused these recent years in the main risk factors for genitourinary prolapse. Vaginal delivery has been recognized for years as the essential risk factor of developing a pelvic organ prolapse [2]. In fact, injuries of supportive, muscular and nervous structures occur mainly during the second phase of labor, when the foetal head distends and crushes the pelvic floor [3]. According to Jelovsek et al. study [4], the relative risk of developing a pelvic organ prolapse is 8.4 for a woman who gave birth twice vaginally compared to a nulliparous and 10.9 for four vaginal deliveries or more. The authors also showed that each vaginal delivery represents a risk of 10% to 20% aggravation of the POP [4]. We can then consider not only vaginal delivery as a main risk factor, but also multiparity. Our first patient is a very good example because she has had numerous vaginal deliveries. Consistent with Jelovsek et al. study [4], her risk of developing a cystocele was 20.9 to 30.9, which occurred at the age of 49. However, large-scale epidemiological studies like Nygaard et al. [5] showed the presence of prolapse in women having undergone a caesarean section and the authors assume that caesarean delivery can reduce the risk of pelvic organ prolapse comparing to the vaginal delivery but does not prevent it completely. Therefore these findings should not be used to justify an increase in the use of caesarean sections. Besides the delivery mode, the pregnancy itself can be considered as a risk factor of developing a cystocele. Recent studies have found the presence of a stage II cystocele in 24% to 40% of nulliparous women during their first pregnancy, while no woman in the population control showed POP [6,7]. Furthermore, a worsening of POP during pregnancy has been described and the persistence in the postpartum was more common among patients who gave birth vaginally [8]. The role of hormone replacement therapy is very controversial. Lukacz et al. [9] found a link between the risk of POP and postmenopausal hormone replacement therapy whereas other authors such as Nygaard et al. or Swift et al. [5,10] have conducted studies with multivariate statistical analyses and find no significant between them. Therefore, we suggest not considering hormone replacement therapy as a risk factor of POP. Prospective randomized studies seem necessary to clarify this situation. Our second patient did not have any of the obstetric factors studied previously. Non-obstetric risk factors are also relevant and they can be divided into three categories: the lifestyle factors, the comorbidities and finally the unmodifiable ones. Among the lifestyle factors, we can study the body mass index. Swift et al. [11] and Whitcomb et al. [12] showed us that the higher the body mass index, the greater the risk of developing a cystocele. Other lifestyle factors have been studied such as smoking and physical activity but the results were inconsistent [13,14]. Diabetes mellitus, chronic illness and previous hernia surgery were studied in Italy, and only diabetes mellitus was significantly associated with primary pelvic organ prolapse [15]. Finally, it is important to remember the non-modifiable risk factors. Age is considered as one of the main risk factor [16]. There are no studies that significantly highlight race or ethnicity as a risk factor. We can then consider that our second case had some important factors other than the obstetric risk factors suchlike obesity, age and diabetes mellitus. In the light of this data, despite the fact that both patients presented the same pathology, their pathophysiological records were different. Although we cannot exactly trace the mechanisms that led to the cystocele, we can assume that for the first one, the major factor was her multiparity and her numerous vaginal deliveries; as for the second patient, her age, her diabetes mellitus and especially her obesity played a significant role in the appearance of her advanced cystocele.
Conclusion
Through this work we hope to inform the general public about this pathology that is a source of important functional disorders in women and could in some cases be the cause of a social discomfort and tensions within the couple. Finally, it is essential to highlight that non-obstetric risk factors that can be modified or controlled can provide an effective primary prevention ground.
REFERENCES
- Dietz HP. The aetiology of prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(10):1323-29.
- Ragni E, Haab F, Delmas V, et al. Physiopathology of genitourinary prolapse. Progrès En Urologie. 2009;19(13):926-31.
- Dietz HP, Lanzarone V. Levator trauma after vaginal delivery. Obstet Gynecol. 2005;106(4):707-12.
- Jelovsek JE. Pelvic organ prolapsed. Lancet.2007;369:1027-38.
- Nygaard I, Bradley C, Brandt D. Pelvic organ prolapse in older women: Prevalence and risk factors. Obstet Gynecol. 2004;104(3):489-97.
- O’Boyle AL, Woodman PJ, O’Boyle JD, et al. Pelvic organ support in nulliparous pregnant and nonpregnant women: A case control study. Am J Obstet Gynecol. 2002;187(1):99-102.
- Sze EH, Sherard III GB, Dolezal JM, et al. Pregnancy, labor, delivery and pelvic organ prolapse. Obstet Gynecol. 2002;100(5):981-6.
- O’Boyle AL, O’Boyle JD, Calhoun B, et al. Pelvic organ support in pregnancy and postpartum. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(1):69-72.
- Lukacz ES, Lawrence JM, Contreras R, et al. Parity, mode of delivery and pelvic floor disorders. Obstet Gynecol. 2006;107(6):1253-60.
- Swift SE. The distribution of pelvic organ support in a population of female subjects seen for routine gynecologic health care. Am J Obstet Gynecol. 2000;183(2):277-85.
- Swift S, Woodman P, O'Boyle A, et al. Pelvic Organ Support Study (POSST): The distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol. 2005;192(3):795-806.
- Whitcomb EL, Rortveit G, Brown JS, et al. Racial differences in pelvic organ prolapse. Obstet Gynecol. 2009;114(6):1271-77.
- Slieker-ten Hove MC, Pool-Goudzwaard AL, Eijkemans MJ, et al. Prediction model and prognostic index to estimate clinically relevant pelvic organ prolapse in a general female population. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(9):1013-21.
- Kudish BI, Iglesia CB, Gutman RE, et al. Risk factors for prolapse development in white, black, and hispanic women. Female Pelvic Med Reconstr Surg. 2011;17(2):80-90.
- Parazzini F, De Aloysio D, Di Donato P. Risk factors for genital prolapse in non-hysterectomized women around menopause: Results from a large cross-sectional study in menopausal clinics in Italy. Eur J Obstet Gynecol Reprod Bio. 2000;93(2):135-40.
- Vergeldt TF, Weemhoff M, IntHout J, et al. Risk factors for pelvic organ prolapse and its recurrence: a systematic review. Int Urogynecol J. 2015;26(11):1559-73.