Understanding lymphedema: pathophysiology and implications for clinical management
Received: 03-Sep-2023, Manuscript No. puljpl-23-6817; Editor assigned: 07-Sep-2023, Pre QC No. puljpl-23-6817 (PQ); Accepted Date: Sep 27, 2023; Reviewed: 23-Sep-2023 QC No. puljpl-23-6817 (Q); Revised: 26-Sep-2023, Manuscript No. puljpl-23-6817 (R); Published: 29-Sep-2023
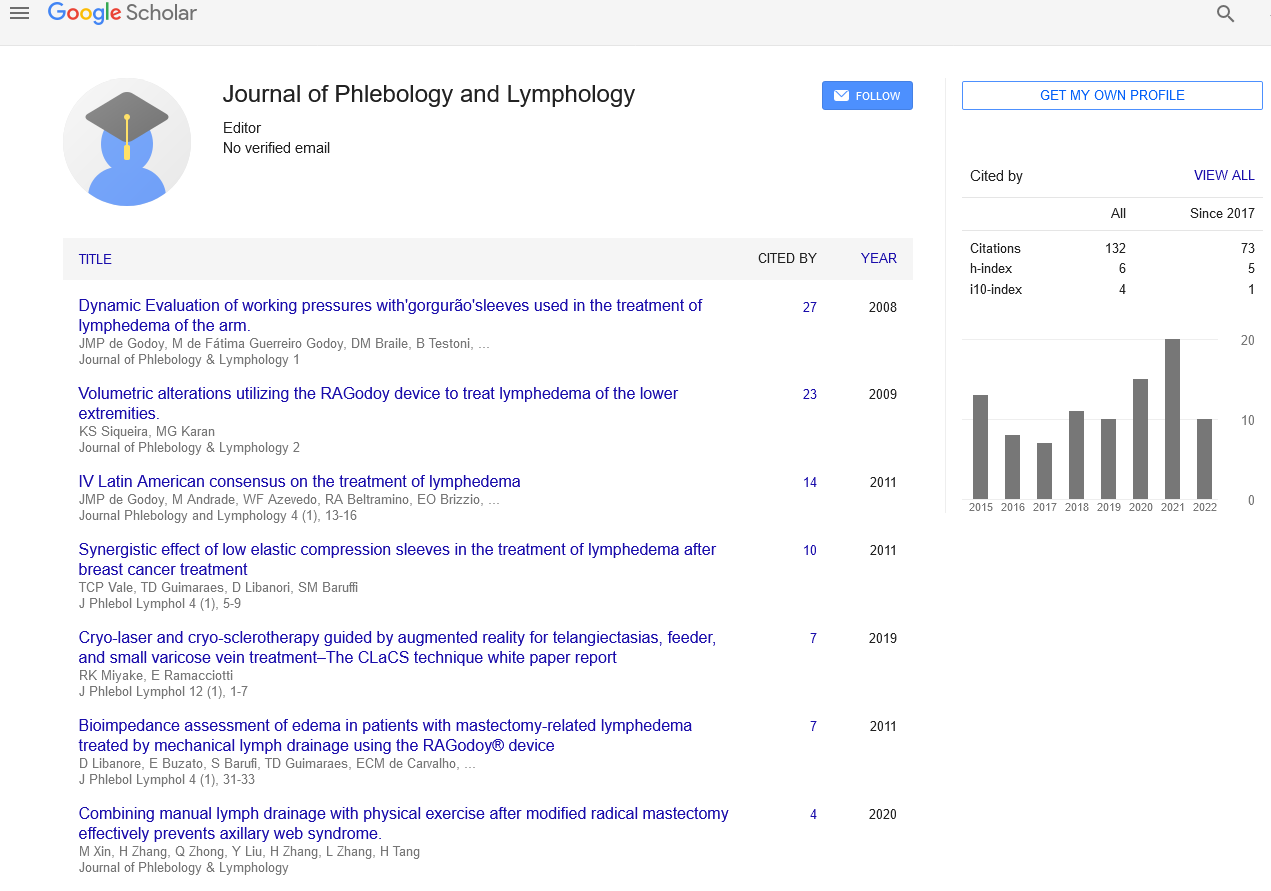
Citation: Angelou M. Understanding lymphedema: pathophysiology and implications for clinical management. J Phlebol Lymphology. 2023; 16(3):1-2.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Lymphedema is a chronic and progressive condition characterized by abnormal accumulation of lymphatic fluid, leading to swelling and tissue changes. The pathophysiology of lymphedema involves
disruptions in the lymphatic system, including impaired lymphatic drainage and inflammation. This article provides an in-depth exploration of the pathophysiological mechanisms underlying lymphedema and discusses their relevance for clinical management. Understanding the intricate molecular and physiological processes involved in lymphedema is crucial for the development of effective therapeutic strategies.
Key Words
Lymphedema; Pathophysiology; Lymphatic system
Introduction
Lymphedema is a chronic and debilitating condition that affects millions of individuals worldwide. It results from the accumulation of protein-rich lymphatic fluid in the interstitial spaces due to impaired lymphatic circulation and drainage. The lymphatic system plays a vital role in maintaining tissue homeostasis and immune function. Disruption of this system can occur due to various factors, leading to the development of lymphedema. The pathophysiology of lymphedema is complex and multifaceted, involving a cascade of events that contribute to the progression and manifestation of the disease. Understanding these underlying mechanisms is essential for advancing treatment modalities and improving the quality of life for individuals suffering from lymphedema. Primary lymphedema is often a result of congenital abnormalities or developmental malformations of the lymphatic system. It can manifest at birth, during adolescence, or later in adulthood. Genetic mutations affecting lymphatic vessel development or function are often implicated in primary lymphedema. These mutations disrupt the normal growth and organization of lymphatic vessels, leading to impaired lymphatic drainage and subsequent fluid accumulation in tissues.above heart level promotes drainage and minimizes edema Regular monitoring of the edema, wound healing, and patient progress is vital. Prompt follow-up appointments allow healthcare providers to assess the progress and adjust the management plan accordingly. Antiinflammatory medications prescribed by the surgeon can help manage postoperative inflammation and associated discomfort. Gentle exercises and mobility-enhancing activities guided by a physical therapist can assist in promoting blood circulation and reducing edema. Gradual movement helps prevent stiffness and discomfort. Secondary lymphedema is more common and occurs as a consequence of damage to the lymphatic system. This damage can be a result of surgery, radiation therapy, trauma, infection, or malignancies such as lymphomas or metastatic cancers. Surgical interventions involving the removal or damage to lymph nodes and radiation therapy can cause scarring and fibrosis, obstructing lymphatic flow and causing lymphedema. Infections can also lead to inflammatory responses that damage lymphatic vessels and hinder proper lymphatic drainage.
In both primary and secondary lymphedema, the disrupted lymphatic circulation results in the accumulation of lymphatic fluid within the affected tissues. The stagnant fluid leads to increased interstitial pressure and triggers an inflammatory response, further exacerbating tissue damage. Chronic inflammation and tissue fibrosis contribute to the progression of the disease, causing irreversible changes in the affected areas.
Clinical Implications and Management
Understanding the pathophysiology of lymphedema is critical for effective clinical management. While lymphedema is currently considered incurable, various treatments aim to mitigate its symptoms, prevent progression, and improve patients' quality of life. The management of lymphedema typically involves a multidisciplinary approach that includes lymphatic drainage techniques, compression therapy, exercise, skin care, and, in some cases, surgical interventions.
Lymphatic drainage techniques, such as manual lymphatic drainage and complete decongestive therapy, are cornerstone treatments that focus on redirecting lymphatic fluid and reducing swelling. Compression therapy, through the use of compression garments or bandages, helps to maintain reduced limb volume and supports lymphatic flow. Exercise, particularly tailored to individual capabilities and conditions, aids in promoting lymphatic circulation and muscle pump activity.
Conclusion
Lymphedema is a chronic condition characterized by abnormal accumulation of lymphatic fluid, resulting from disruptions in the lymphatic system. The pathophysiology of lymphedema involves impaired lymphatic drainage, inflammation, and tissue fibrosis. Understanding these underlying mechanisms is crucial for the development of targeted therapeutic strategies. While lymphedema remains incurable, a multidisciplinary approach to clinical management focusing on lymphatic drainage techniques, compression therapy, exercise, and skin care can significantly improve the quality of life for individuals living with this condition. Further research and advancements in treatment modalities are essential to enhance our understanding and provide better outcomes for those affected by lymphedema..