Unescorted clinic visits: Practical consequences of a stressor imposed by the COVID-19 pandemic
2 Department of Ophthalmology, University of Patras Medical School, Patras, Greece, Email: pbpolitis@gmail.com
Received: 02-Aug-2021 Accepted Date: Aug 16, 2021; Published: 23-Aug-2021
Citation: Tranos PG, de Politis, Vasileiou D, et al. Unescorted clinic visits: Practical consequences of a stressor imposed by the COVID-19 pandemic. Curr Res Integr Med. 2021;6(2): 7-10.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: One of the restrictive measures of COVID-19 (Coronavirus Disease 2019) pandemic control is the prohibition of escorted clinic visits. Ophthalmological patients’ specific features imply different degrees of dependency, directly affecting their response to such quarantine impositions. This study aims to assess the effects of unaccompanied medical appointments in outpatients’ stress level and absorption of medical advice.
Methods: A questionnaire-based survey was conducted in a large ophthalmic service in Northern Greece during September 2020. Suitable subjects were requested to self-administer a 7-item questionnaire addressing subjective perception of stress and their ability to fully understand and recall doctor’s instructions, considering eye examination in the absence of an escort.
Results: Analysis was based on two hundred consecutive patients who completed the survey. Sixty-three patients (31.5%) reported unescorted clinic visits increasing stress, with a median value of 7.5 (mean 6.77 ± 2.7) in a scale from 1 to 10. A large proportion of patients (30%) claimed difficulty recalling doctor’s comments or instructions and 24.6% anticipated not fully understanding them, should they attend the clinic unaccompanied. Patients living in smaller towns report the highest stress levels (p=0.002) when attending the clinic alone. A marked impact on women and the elderly above 70 years (up to threefold) was identified.
Conclusion: This is the first study specifically addressing practical repercussions of unescorted clinic visits during COVID-19 pandemic. A negative effect on patients’ emotional status and counseling effectiveness was demonstrated. Female gender and advanced age were found as determinants of the highest vulnerability.
Keywords
COVID-19; Ophthalmology; Impact; Psychological distress
Introduction
Following the SARS-CoV-2 (Severe-Acute-Respiratory-Syndrome-Corona- Virus-2) pandemic, several contention rules have been issued by national governments worldwide in the attempt to limit virus spread and increase safety conditions both for patients and health providers. One of the restrictive measures imposed on public and private medical centers is the prohibition of escorts inside facilities. Although clinical examination per se remains unchanged, unescorted appointments have been a challenging matter, with potential impact on effective counseling and patients’ psychological status.
This study aims to investigate the effects of unescorted clinic visits on patients’ stress level and to explore its impact on counseling effectiveness. A segmental analysis was conducted on collected data, in order to identify patient groups more susceptible to be negatively affected by the absence of escorts during eye examination.
Materials and Methods
This is a prospective questionnaire-based study involving subjects who attended ophthalmologic examination at the Ophthalmica Eye Institute, in Thessaloniki, during September 2020, at the beginning of the second pandemic wave in Greece. The study was approved by the facility’s Ethics Committee and a written informed consent was obtained from each eligible participant.
Eligibility criteria included minimum age of 17 years, fluently reading Greek and passing a brief version of the Folstein Mini-Mental State examination, comprised by orientation, registration, and attention and calculation questions [1]. Suitable subjects were requested to self-administer a 7-item questionnaire assessing subjective perception of stress, as brought by the absence of an escort during eye examination. Moreover, the survey addressed patients’ anticipation of the ability to fully understand and recall doctor’s instructions or to have all queries answered without the aid of an escort. Individuals were also asked whether unescorted clinical visits could imply less than required appointments or better protection of personal health data (Appendix). Research staff described the questionnaire and gave verbal instructions and assistance when needed. Upon completion, the survey was reviewed for missing data and returned to the patients for final filling prior to the consultation.
Box-and-whisker plots and histograms were used to summarize distributions. Parametric methods, including independent t-test, ANOVA and linear regression, were applied to normally distributed variables. Non-parametric tests, such as Mann-Whitney U and Wilcoxon-signed rank tests were performed for variables showing non-normality. Correlations between questionnaire scores and patients’ demographics or characteristics like social status, attendance history and reason for visiting were examined by Pearson and Spearman rank correlation tests. Relationships between categorical variables were evaluated through chi-squared tests. Subgroup analysis was conducted to identify individuals more susceptible to negatively experience the absence of escorts during eye examination. All tests of association were considered statistically significant at p<0.05. Analyses were conducted by using SPSS (version 20.0, SPSS, Chicago, IL, USA).
Results
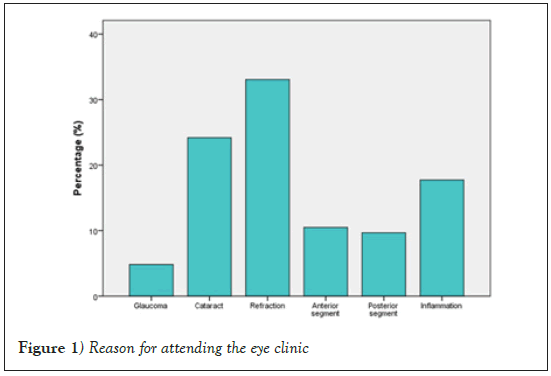
Studied sample consisted of two hundred consecutive patients who completed the questionnaire, of which 49% were male and 51% female. Mean age was 45.04 years. In 25 cases (12.5%), research staff noticed missing data and instructed patients to fill in omitted answers. Table 1 summarizes general characteristics of the enrolled subjects. One hundred fourteen patients (57%) were residents of Thessaloniki, a city with a 1.1-million population, whereas the remaining 86 (43%) lived in smaller towns or villages. Most subjects (82%) declared sharing the house with family, while 18% were living alone. Regarding frequency of clinic visits, forty-four percent were first- time patients, 33% had attended 1 to 3 visits, 14% 4 to 10 visits and 9% had attended the clinic over 10 times. Figure 1 categorizes their reason for attendance.
| Sex | |
|---|---|
| Male | 98 (49%) |
| Female | 102 (51%) |
| Age (years) | |
| Range | 18-86 |
| Mean (SD) | 45.04 (18.6) |
| Place of residence | |
| City (>1 million population) | 115 (57.3%) |
| Town or village | 85 (42,7%) |
| Single person household | |
| Yes | 36 (18.1%) |
| No | 164 (81.9%) |
| Number of previous visits | |
| 0 | 88 (44.3%) |
| 1-3 | 66 (32.8%) |
| 3-10 | 28 (14.1%) |
| >10 | 18 (8.9%) |
Table 1: General characteristics of enrolled subjects (200 patients)
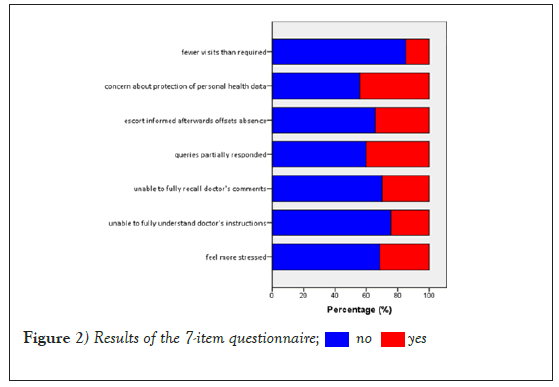
Questionnaire results are displayed in Figure 2. Sixty-three patients (31.5%) reported that unescorted clinic visits caused them more stress. When scoring stress level in a scale from 1 to 10, subjects rendered a median value of 7.5 (mean 6.77 ± 2.7). A large proportion of patients (30%) claimed difficulty recalling doctor’s comments or instructions and 24.6% anticipated not fully understanding them, should they attend the clinic unaccompanied.
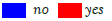
Subgroup analysis revealed that patients living in smaller towns report the highest stress levels (p=0.002), tendency to forget doctor’s recommendations (p<0.001), trouble absorbing information delivered during consultation (p=0.019) and leaving with unsettled questions (p=0.02) for having no escorts. Female patients are more likely to feel stressed (p=0.009) and fail to resolve all their queries (p=0.04) when attending the clinic alone. Figure 3 illustrates stress response to unescorted visit by gender.
When the reason for visiting was tested as a determinant, results revealed that subjects attending for cataract, as opposed to refractive surgery (p=0.002) or uveitis (p=0.025), were more severely affected by the absence of an escort. However, this finding lost significance (p>0.5) once multivariate analysis was performed, using age and gender as covariates.
To 40% of patients, the presence of an escort would facilitate having their queries fully responded, while 65% asserted that escorts being informed later by the doctor cannot counterbalance their absence during consultation. More than half of subjects (55%) were unconcerned about the personal health data disclosure inherent to escorted visits. Although only 15% of patients consider visiting the clinic less frequently than required due to the absence of a companion, this index escalates up to 55% in the oldest groups.
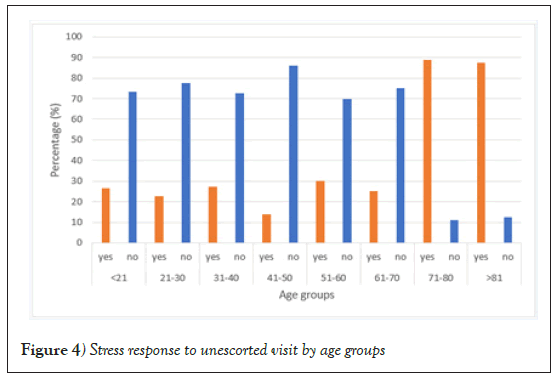
Undoubtedly, the impact of unescorted clinic visits is more evident in older patients, who do not only display more psychological distress (p=0.004) and less understanding of the consultation (p=0.002), but also are more prone to forget things said by the doctor (p=0.005) and to attend the clinic fewer times than required (p=0.002) for being unaccompanied. Further analysis of age groups revealed that this impact is threefold for patients older than 70 years, when compared to younger individuals. Figure 4 depicts stress response to unescorted visit by age groups.
Discussion
As early as mid-September 2019, the World Health Organization published a series of guidelines to help protect health workers and patients from the spread of SARS-CoV-2. All over the world, medical facilities of every complexity level, including eye clinics, have adhered to restrictive measures and made adaptations in order to ensure safe continuity of medical assistance [2-12]. As shown by numerous publications in medical literature, nationwide quarantine impositions cause negative psychological effects, increasing stress among the population [13-29].
The study presented herein is a questionnaire-based survey assessing direct implications of unescorted clinic visits on effective counseling and patients’ emotional status. Results are consistent with most findings cited in reports regarding psychological distress caused by the SARS-CoV-2 pandemic and spread-contention rules imposed by national governments [14-29].
Along with the physiological stress naturally embedded in a medical visit, for being examined, discussing illness and possibly undergoing a procedure, patients living the pandemic fear getting infected while commuting or staying in the clinic. Attending appointments unaccompanied adds to their sense of vulnerability, increasing their stress level.
In general, our results show that unescorted clinic appointments, as part of the restrictive measures applied by public administration during the COVID-19 pandemic, are a stress trigger for nearly one-third of patients.
Up to 40% of subjects, regardless of gender or age, feel that the absence of an escort makes it more difficult for them to understand and retain medical counseling, a fact that may have serious consequences to the actual practice, compromising therapeutic effectiveness and making the entire visit pointless. To approximately two-thirds of patients, their escorts getting a later report of the visit does not compensate for not being present during consultation, a strong indicator of the importance of a third-party presence in the completion of the visit’s goal.
Considering the advantage of privacy preservation, more than half of patients are not concerned about having their medical records exposed to their escorts. When looking at the results on effective counseling, it is possible to infer that most of them prefer to share their health data in order to ensure recollection of doctor’s recommendations.
Cultural and social backgrounds play an important role in the impact of restrictive measures on patients’ welfare and effective advice. Living in the city facilitates attending clinic visits regardless of the presence of an escort. Inhabitants of big cities are usually more independent, while those living in smaller towns tend to have closer relationships with their fellows, which most certainly explain their higher stress level associated with unescorted appointments.
The nature of eye condition seems to play an important role in limiting unaccompanied trips to the doctor. Of all individuals who claim they come to the clinic less often for having no escort, half (50%) have cataract. It is possible to assume that a higher degree of dependence due to age and visual impairment makes it more difficult to adhere to a medical schedule without an escort. On the other hand, cataract rarely needs urgent intervention; therefore, patients may prefer waiting until they can be escorted at their appointments.
Despite the negative impact brought by the prohibition of escorts inside medical facilities, most patients comply with their clinical schedule. Notably, those who live with others do not miss their appointments, even if their escort must wait outside. Subgroup analysis showed that, of the 15% who limit excursions to the clinic because of being unaccompanied, over twothirds are women and elderly, implying that age and gender are the two isolated factors significantly affecting patients’ decision to attend medical consultation in the case of having no escort.
Despite the approximately equal gender distribution in the studied sample, female higher predisposition to stress under the considered situation is clearly statistically significant. Women also show more difficulty solving their queries in the absence of an escort. Our results are in accordance with published literature on the psychological distress caused by pandemic and quarantine, showing greater impact on women, confirming the influence of gender in the emotional response to such conditions [14,16-29].
A few of these studies also signal age as an important factor determining pandemic stress level [15,17-29]. According to our survey, advanced age has the most overall significant impact on patients’ emotional response to the absence of an escort during medical visits. Older patients do not only experience the highest stress levels under such restriction, but also have the greatest difficulty understanding and recalling medical advice. Furthermore, they are the ones with the highest tendency to pay fewer visits to the clinic than they normally would, just for being unescorted.
We acknowledge as limitations of our study its relatively small sample size and the reliance on a non-validated questionnaire. However, the survey was developed to address patients’ subjective perception of unescorted clinic visits, focusing on psychological issues and potential practical consequences. The prospective design of the investigation provides a comprehensive overview of difficulties met by patients when attending eye clinics unaccompanied.
To the best of our knowledge, this is the first study assessing pandemic stress level specifically related to unescorted clinic visits and the implications of such imposition on effective medical advice. Results clearly show that older patients are the most affected by the prohibition of escorts during medical consultation, notably those above 70 years of age. Given the potential hazards to clinical practice and patients’ welfare, we propose an age-related exception to this quarantine rule, for the benefit of the elderly in that range.
Conclusion
COVID-19 pandemic has affected basic life routines in unimaginable ways for the living generations. Unescorted clinic visits, as part of the restrictive measures imposed by national governments to limit virus spread, have a negative impact on patients’ emotional status and may compromise counseling effectiveness. Alternatives must be found to minimize psychological distress and ensure proper retention of medical advice to patients living the pandemic who need to attend health facilities.
Declarations
Funding
The authors have NO funding to report.
Conflicts of interest/competing interests
The authors certify that they have NO affiliations with or involvement in any organization or entity with any financial or non-financial interest in the subject matter or materials discussed in this manuscript.
Availability of data and material
All 200 questionnaires as filled by the subjects involved in this survey were digitalized and available upon request.
Code availability
Not applicable.
Author’s contribution
PT, PP and DV contributed to the conception and design of the work, the acquisition, analysis or interpretation of data. MB, EL, SA, VV and PS contributed to revising the manuscript critically for important intellectual content. All authors are responsible for the final approval of the version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethics approval
Ethics approval was obtained from the Ophthalmica Eye Institute Ethics Committee, under reference number 102020/004.
Consent to participate
A written consent was obtained from all subjects participating in this survey.
Consent for publication
This manuscript does not contain personal data from any individual person. All authors consent to the publication of the manuscript in Health Care Management Science.
REFERENCES
- Folstein MF, Folstein SE, McHugh PR. (1975). Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. J Psychiatric Res. 1975;12(3): 189-198.
- Gegúndez-Fernández JA, Zarranz-Ventura J, Garay-Aramburu G, et al. Recommendations for eye care during the alarm state by the coronavirus disease pandemic COVID-19. Archivos de la Sociedad Espanola de Oftalmologia. 2020; 95(6): 300-310.
- Cheung S, Wong C, Chan J, et al. Ophthalmology in the time of COVID-19: Experience from Hong Kong eye hospital. International J Ophthalmol. 2020;13(6): 851-859.
- Romano MR, Montericcio A, Montalbano C, et al. Facing COVID-19 in ophthalmology department. Current Eye Res. 2020;45(6): 653-658.
- Veritti D, Sarao V. Infection control measures in ophthalmology during the COVID-19 outbreak: A narrative review from an early experience in Italy. Eur J Ophthalmol. 2020;30(4): 621-628.
- Singh P, Müller M, Hack D, et al. Development and implementation of an operational concept in a university eye hospital in the SARS-CoV-2 pandemic. 2020;117(7): 595-601.
- Borrelli E, Sacconi R, Querques L, et al. Taking the right measures to control COVID-19 in ophthalmology: The experience of a tertiary eye care referral center in Italy. Eye. 2020;34(7): 1175-1176.
- Lim LW, Yip LW, Tay HW, et al. Sustainable practice of ophthalmology during COVID-19: Challenges and solutions. Graefe's Archive Clin Exp Ophthalmol. 2020;258(7): 1427-1436.
- Babu N, Kohli P, Mishra C, et al. To evaluate the effect of COVID-19 pandemic and national lockdown on patient care at a tertiary-care ophthalmology institute. Indian J Ophthalmol. 2020;68(8): 1540-1544.
- Danesh-Meyer HV, McGhee C. Implications of coronavirus disease 2019 for ophthalmologists. American J Ophthalmol. 2020;223:108-118.
- Bourdon H, Jaillant R, Ballino A, et al. Teleconsultation in primary ophthalmic emergencies during the COVID-19 lockdown in Paris: Experience with 500 patients in March and April 2020. Journal Francais d'Ophtalmologie. 2020;43(7): 577-585.
- Arrigo A, Aragona E, Parodi MB, et al. Ophthalmology and SARS-CoV-2: Blind toward those who fight blindness? European J Ophthalmol. 2020;30(5): 1185-1187.
- Moreno C, Wykes T, Galderisi S, et al. How mental health care should change as a consequence of the COVID-19 pandemic. The Lancet Psychiatry. 2020;7(9): 813-824.
- Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in china. Int J Environmental Res Public Health. 2020;17(5): 1729.
- Tian F, Li H, Tian S, et al. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 2020;288: 112992.
- Liu N, Zhang F, Wei C et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. 2020;287: 112921.
- Mazza C, Ricci E, Biondi S, et al. A nationwide survey of psychological distress among italian people during the COVID-19 pandemic: Immediate psychological responses and associated factors. Int J Environmental Res Public Health. 2020;17(9): 3165.
- Wang Y, Di Y, Ye J, et al. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med. 2020;26(1): 13-22.
- Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J Psychiatry. 2020;51: 102076.
- Gómez-Salgado J, Andrés-Villas M, Domínguez-Salas S, et al. Related Health Factors of Psychological Distress During the COVID-19 Pandemic in Spain. Int J Environmental Research Public Health. 2020;17(11): 3947.
- Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. The Lancet Psychiatry. 2020;7(10): 883-892.
- Solomou I, Constantinidou F. Prevalence and predictors of anxiety and depression symptoms during the covid-19 pandemic and compliance with precautionary measures: Age and sex matter. Int J Environmental Research Public Health. 2020;17(14): 4924.
- Alkhamees AA, Alrashed SA, Alzunaydi AA, et al. The psychological impact of COVID-19 pandemic on the general population of Saudi Arabia. Comprehensive Psychiatry. 2020;102: 152192.
- Paz C, Mascialino G, Adana-Díaz L, et al. Behavioral and sociodemographic predictors of anxiety and depression in patients under epidemiological surveillance for COVID-19 in Ecuador. PloS One. 2020;15(9): e0240008.
- Torales J, Ríos-González C, Barrios I, et al. Self-perceived stress during the quarantine of COVID-19 pandemic in paraguay: An exploratory survey. Frontiers Psychiatry. 2020;11: 558691.
- Jacques-Aviñó C, López-Jiménez T, Medina-Perucha L, et al. Gender-based approach on the social impact and mental health in Spain during COVID-19 lockdown: A cross-sectional study. BMJ Open. 2020;10(11): e044617.
- Hammarberg K, Tran T, Kirkman M, et al. Sex and age differences in clinically significant symptoms of depression and anxiety among people in Australia in the first month of COVID-19 restrictions: A national survey. BMJ Open. 2020;10(11): e042696.
- García-Álvarez L, de la Fuente-Tomás L, García-Portilla MP, et al. Early psychological impact of the 2019 coronavirus disease (COVID-19) pandemic and lockdown in a large Spanish sample. J Global Health. 2020;10(2): 020505.
- Burhamah W, AlKhayyat A, Oroszlányová M, et al. The psychological burden of the COVID-19 pandemic and associated lockdown measures: Experience from 4000 participants. J Affective Disorders. 2020;277: 977-985.