Unilateral persistent sciatic artery
Received: 08-Jun-2018 Accepted Date: Jun 20, 2018; Published: 30-Jun-2018, DOI: 10.37532/1308-4038.18.11.70
Citation: Kar R, Devorah CM, Barron CI, et al. Unilateral persistent sciatic artery. Int J Anat Var. 2018;11(2):70-72.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Persistent Sciatic Artery (PSA) is a rare congenital vascular anomaly of clinical significance. Sciatic artery persists as a continuation of the internal iliac artery and functions as the major blood supply for the lower limb in rare cases such as the one presented here. Reported here is a unilateral presentation of a persistent sciatic artery (PSA) which continued into the popliteal fossa and divided into the anterior and posterior tibial arteries and gave off genicular branches. The femoral artery (superficial femoral artery) was hypoplastic, and did not reach the popliteal fossa. In addition to the presence of the PSA, bilateral variations in the course of femoral and the profunda femoris veins are reported.
Keywords
Persistent Sciatic artery; Femoral artery; Profunda femoris vein; Femoral vein
Introduction
Persistent sciatic artery (PSA) was first described by Green et al. [1] in a post-mortem case. PSA is a rare embryological malformation, with a prevalence in 0.03-0.06% of the population. It was found to be bilateral in about 32.2% of patients [2]. Most reported PSA cases are found once symptomatic while the asymptomatic presentations are found incidentally.
The sciatic artery, a branch from the umbilical artery is the major source of blood supply to the primitive foot at the 9 mm stage of development. The femoral artery develops as a continuation of the external iliac artery at the 10 mm stage, eventually enlarges and at about the 14mm-stage the lower extremity receives blood supply from both the femoral and the sciatic arteries. The sciatic artery then regresses and the femoral system takes over the blood supply of the lower extremity [3]. However, developmental errors may lead to incomplete development of the femoral artery and persistence of the sciatic artery as a continuation of the internal iliac artery.
This report describes a case of a PSA in a 68-year-old female. In addition to the presence of a complete PSA unilaterally, bilateral variations in the course of the femoral and the profunda femoris veins were also observed.
Results
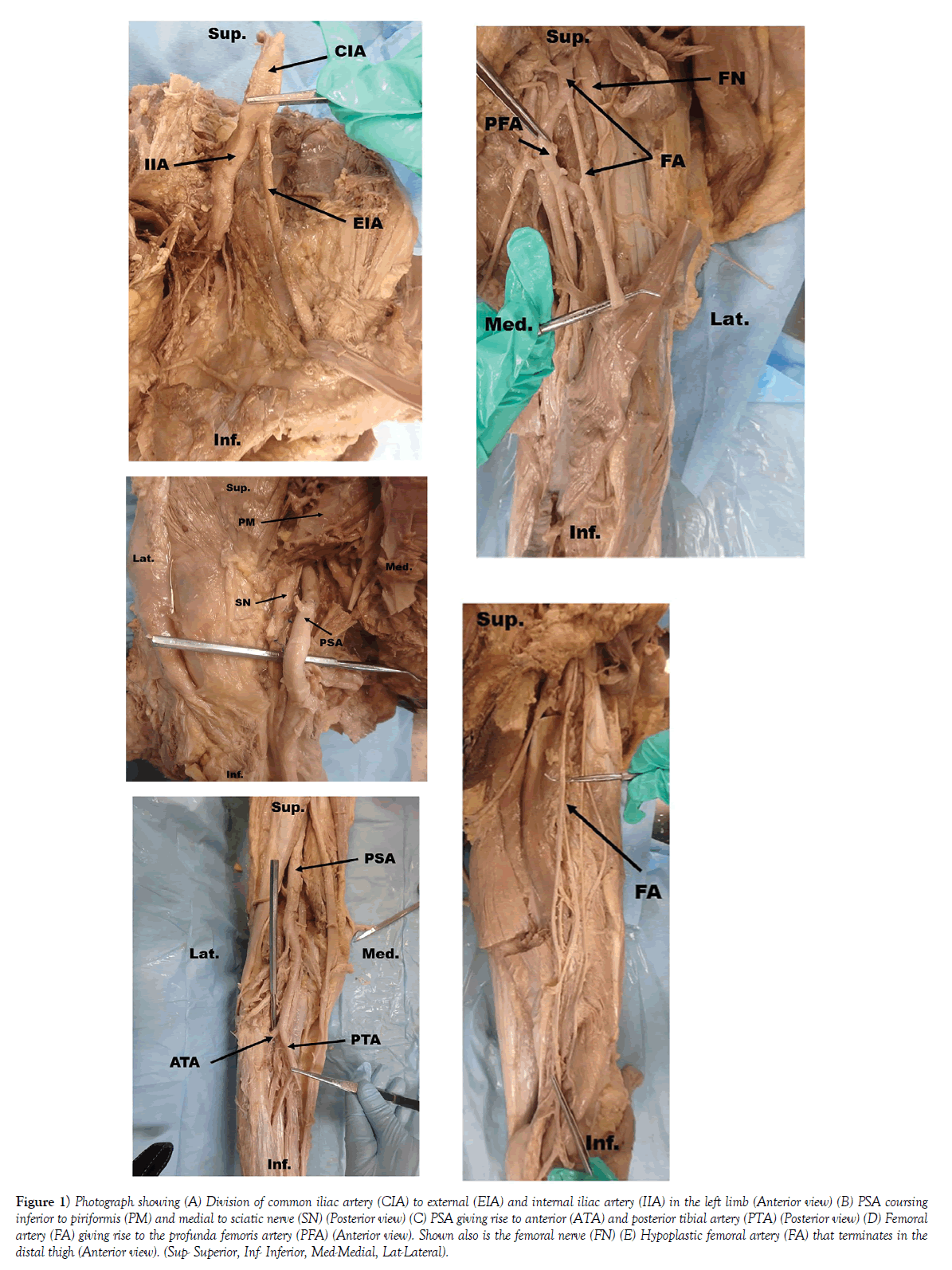
While conducting a routine lower extremity dissection of a left lower limb for second year medical student education, a large aberrant artery coursing inferior to the piriformis muscle was observed. The artery was traced proximally to elucidate its origin and was found to be a continuation of a major branch of the internal iliac artery (Figure 1A). This artery passed through the greater sciatic foramen, inferior to the piriformis muscle and medial to the sciatic nerve (Figure 1B). It then continued inferiorly into the posterior compartment of the thigh. Based on prior publications, this aberrant artery was identified as a PSA. In its descent, the PSA provided branches to all muscles within the posterior compartment of the thigh: the semitendinosus, semimembranosus and the biceps femoris. PSA in this cadaver was complete, reaching the popliteal fossa and giving off genicular arteries. In the popliteal region, the PSA terminated into the anterior and posterior tibial arteries (Figure 1C).
Figure 1) Photograph showing (A) Division of common iliac artery (CIA) to external (EIA) and internal iliac artery (IIA) in the left limb (Anterior view) (B) PSA coursing inferior to piriformis (PM) and medial to sciatic nerve (SN) (Posterior view) (C) PSA giving rise to anterior (ATA) and posterior tibial artery (PTA) (Posterior view) (D) Femoral artery (FA) giving rise to the profunda femoris artery (PFA) (Anterior view). Shown also is the femoral nerve (FN) (E) Hypoplastic femoral artery (FA) that terminates in the distal thigh (Anterior view). (Sup- Superior, Inf- Inferior, Med-Medial, Lat-Lateral).
In this cadaver, the external iliac artery on the left side was very small in diameter (4 mm) as compared to the internal iliac artery (8 mm). The external iliac artery passed deep to the inguinal ligament, descending through the femoral triangle as the femoral artery. The femoral artery gave off the profunda femoris artery and continued inferiorly (Figure 1D). However, the femoral artery was hypoplastic and did not reach the popliteal fossa, terminating in the distal thigh (Figure 1E). Interestingly, the adductor hiatus was absent in this limb. The right lower limb of this cadaver presented with more typical anatomy. The femoral artery, a continuation of the external iliac artery, entered the adductor canal and exited through the adductor hiatus as the popliteal artery. Thus, the PSA in this cadaver was unilateral.
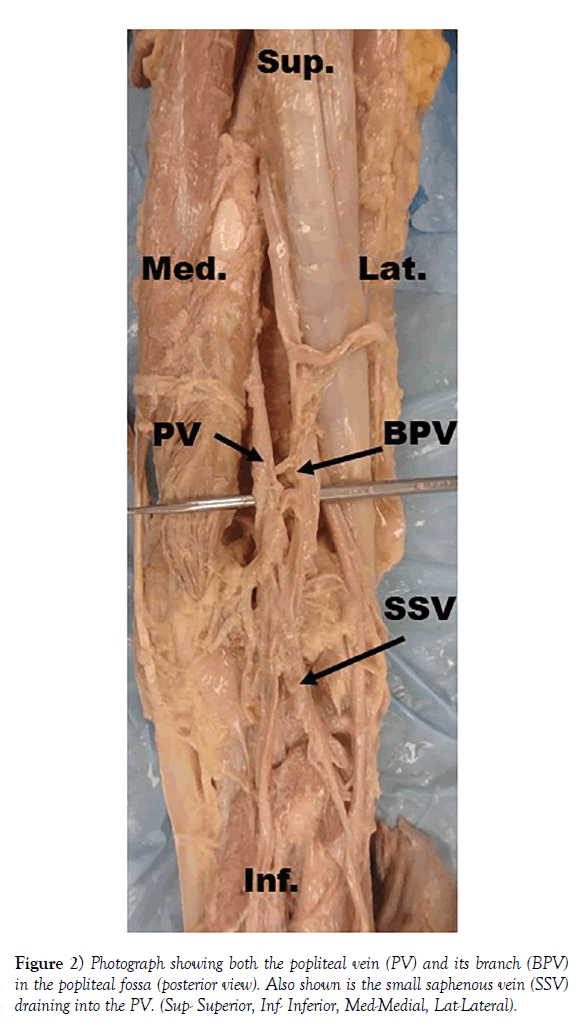
In addition to arterial variation, variations in the major veins were also observed. In the left lower limb, the popliteal vein drained into the profunda femoris vein, not the femoral vein. Superiorly, the profunda femoris vein drained into the femoral vein. Inferiorly, the femoral vein in this limb was hypoplastic, and was not traceable inferior to the knee, similar to the femoral artery. In the right lower limb, the popliteal vein passed through the adductor hiatus to continue superiorly as the femoral vein and a branch from the popliteal vein passed through the adductor magnus to drain into the profunda femoris vein (Figure 2).
Discussion
Even though PSA is a rare embryologic malformation, various classifications for PSA have been described. Pillet et al. [4] classified PSA into 4 different categories: Type I with a complete PSA and a normal femoral artery, type II with a complete PSA and a hypoplastic femoral artery, type III with an incomplete superior PSA, where the upper part of this artery persists along with a completely developed femoral artery and type IV with an incomplete inferior PSA, where the lower part of this artery persists along with the presence of a complete femoral artery. In the complete type (types I and II), the PSA reaches the popliteal fossa and is the main provider of blood to the lower limb. In incomplete PSA (types III and IV), the PSA is usually hypoplastic, ending in the thigh, and the femoral artery continues into the popliteal fossa as the popliteal artery. Based on the classification by Pillet, the PSA in this case report is the complete type (type II) as it reached the popliteal fossa, divided into the anterior and posterior tibial arteries (Figure 1C), and gave off genicular arteries, but the femoral artery was hypoplastic. More recent classification of PSA was published by Ahn et al. [5] based on the presence of complete or incomplete PSA and femoral artery (superficial femoral artery). The present case report fits into the class III type of Ahn- Min’s classification where PSA is complete and femoral artery is incomplete (Figures 1C and E). Ahn et al. [5] reported that PSA is usually seen unilaterally (67.8%) with a slightly higher occurrence on the left side (35.6%) as opposed to the left side (32.2%). PSA in the present case was seen only on the left side.
Interestingly, the diameter of the internal iliac artery (8 mm) in this cadaver was much larger than that of the external iliac artery (4 mm) (Figure 1A), raising the possibility that persistence of the sciatic artery could have been the result of inadequate development of the external iliac artery. Nicholson et al. [6] described two cases of PSA: in one case, both the external iliac artery and femoral artery were completely lacking, and in the other case, both of these arteries were unremarkable. Shah et al. [7] reported persistence of the sciatic artery in a newborn with hypoplastic external iliac artery, which further supports the possibility of incomplete development of the external iliac artery as a contributing factor for failure of the sciatic artery to regress during embryological development.
In this cadaver, the femoral vein in the left lower limb was hypoplastic similar to the femoral artery and the popliteal vein was seen draining into the profunda femoris vein. Reports of such coexistence of venous variations along with PSA are extremely rare. Jiji et al. [8] reported a similar finding in which the popliteal vein communicated directly with the profunda femoris vein; however, these authors did not report any arterial variation (e.g., the persistence of the sciatic artery). Interestingly, the right lower limb which had normal arterial presentation also had venous abnormalities, where the popliteal vein drained both into the femoral vein and the profunda femoris vein. Parry et al. [9] reported PSA in a patient who also had a hypoplastic femoral vein and a persistent sciatic vein that drained into the profunda femoris vein. In the embryo, the sciatic vein runs along with the sciatic nerve, receives venous blood from lower extremity and usually regresses at 10-12 weeks. Similar coexistence of venous variation was also reported by Jung et al. [10] where the limb with PSA had a persistent sciatic vein and a large communicating vein between the profunda femoris vein and the popliteal vein. These authors also reported large communicating veins between the popliteal vein and the profunda femoris vein in the contralateral side without PSA.
In 25-40% of cases of PSA, aneurysms have been reported [11]. Such aneurysms can lead to many other complications such as compression of the sciatic nerve, thrombosis and, in severe cases, loss of limb. Due to the larger than normal size of this artery in the posterior compartment of the thigh, PSA can lead to complications due to compression that occurs in repeated hip flexion (e.g., frequent bending or sitting down). Patients with PSA remain asymptomatic in their early years but begin to exhibit symptoms at the mean age of 40 to 60 years with equal gender preference. Clinical presentation may vary based on whether the PSA is complete / incomplete and the presence or absence of other venous variations as reported in this study. Physicians need to be aware of these possible anatomical variations to appropriately diagnose, treat and advise patients if lifestyle changes are necessary.
REFERENCES
- Green PH. On a new variety of femoral artery. Lancet 1832;1:730-1.
- Van Hooft IM, Zeebregts CJ, Van Sterkenberg SM. The Persistent Sciatic artery. Eur J Vasc Endovasc Surg. 2009;37:585-91.
- Senior HD. The development of the arteries of the lower extremity. Am J Anat 1919;25:55-95.
- Pillet J, Albaret P, Toulemonde JL, et al. Ischio-popliteal artery trunk, persistence of the axial artery. Bull Assoc Anat (Nancy). 1980;64:97-110.
- Ahn S, Min SI, Min SK, et al. Treatment Strategy for Persistent Sciatic Artery and Novel Classification Reflecting Anatomic Status. Eur J Vasc Endovasc Surg. 2016;52:360-9.
- Nicholson R, Pastershank S, Bharadwaj B. Persistent Primitive Sciatic Artery. Radiol. 1977;122:687-9.
- Shah SK, Phan NB, Doshi S, et al. Symptomatic persistent sciatic artery in a newborn. J Pediatric Surg. 2008;43:1741-4.
- Jiji P, D Costa S, Prabhu L, et al. A rare variation of the profunda femoris vein in the popliteal fossa. Singapore Med J. 2007;48:948-9.
- Parry DJ, Aldoori MI, Hammond RJ, et al. Persistent sciatic vessels, varicose veins, and lower limb hypertrophy: An unusual case or discrete clinical syndrome? J Vas Surg. 2002;36:396-400.
- Jung Ah, Lee W, Chung JK, et al. Role of computed tomographic angiography in the detection and comprehensive evaluation of persistent sciatic artery. J Vasc Surg. 2005;42:678-83.
- Ahmad W, Majd P, Luebke T, et al. Clinical outcome after surgical and endovascular treatment of symptomatic persistent sciatic artery with review of the literature and reporting of three cases. Vascular. 2016;24:469-80.