Unilateral variant vertebral artery with an aneurysm of the basilar tip: a case report
Deniz Uzmansel1*, Zeliha Kurtoglu1, Celal Bagdatoglu2, Alev Kara1 and Altan Yildiz3
1Mersin University, Faculty of Medicine, Departments of Anatomy,33169, Mersin, Turkey.
2Mersin University, Faculty of Medicine, Departments of Neurosurgery,33169, Mersin, Turkey.
3Mersin University, Faculty of Medicine, Departments ofNeurosurgery and Radiodiagnostic,33169, Mersin, Turkey.
- *Corresponding Author:
- Deniz Uzmansel, MD
Mersin University, Faculty of Medicine Department of Anatomy, Yenisehir Campus Mersin, 33169,Turkey.
Tel: +90 (324) 3412815/1053
E-mail: duzmansel@yahoo.com
Date of Received: April 9th, 2009
Date of Accepted: August 12th, 2009
Published Online: August 30th, 2009
© IJAV. 2009; 2: 96–98.
[ft_below_content] =>Keywords
basilar artery,aneurysm,vertebral artery,hypoplasia,vertigo
Introduction
Intracranial aneurysms are classified in 3 groups as saccular (berry), fusiform and dissecting aneurysms, regarding their pathological appearance. Among those, saccular ones constitute 90-95% of all cases, and are found at the bifurcation site where the hemodynamic stress is highest [1].
Arterial anatomy of the posterior cranial fossa is variable. It has been already reported that unequal diameters of the vertebral arteries (VA) cause insufficiency in the vertebrobasilary circulation, which in turn results in vertebrobasilary ischemia [2].
Here, the relation between the basilar tip aneurysm and hypoplastic left vertebral artery, as well as the role of the hypoplasia in vertebrobasilar insufficiency etiology are discussed.
Case Report
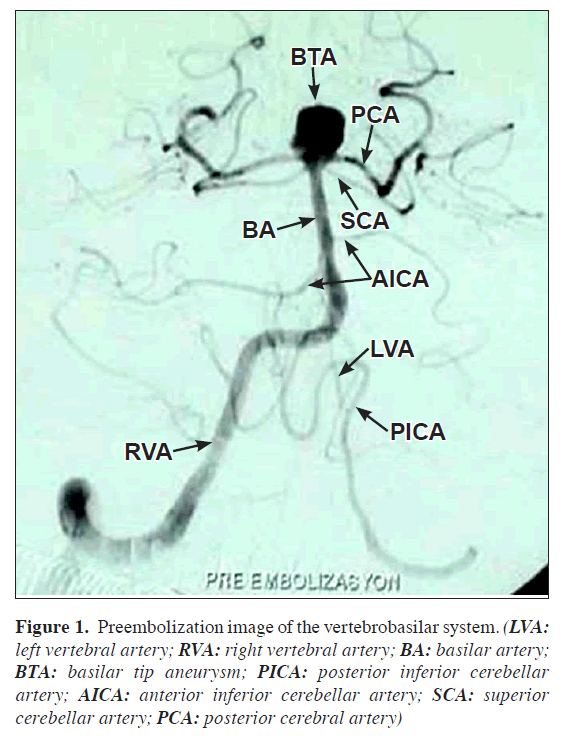
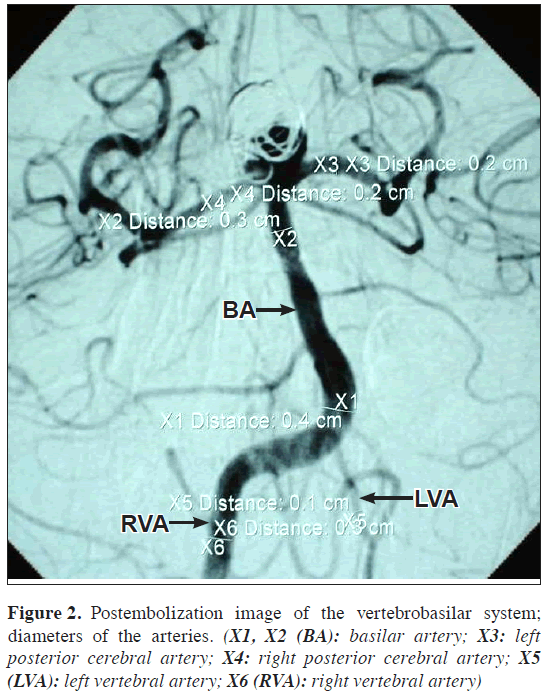
A 45-year-old male patient consulted to a neurosurgeon with headache and vertigo, and a cranial CT revealed an aneurysm at the prepontine cistern. A further cerebral angiography showed the aneurysm at the basilar tip where it divides into two posterior cerebral arteries. A partially hypoplastic left VA was also detected. Basilar artery (BA) was formed by the union of a normal right VA and a partially hypoplastic left VA at the bulbopontine junction, and its diameter was 4 mm. The dimension of the basilar tip aneurysm was 12x13 mm. The lumen diameter of the right VA was 3 mm, the left VA was 1.2 mm and 0.8 mm before and after giving the posterior inferior cerebellar artery (PICA), respectively. The BA was deviated to the hypoplastic side. The hypoplastic part of the left VA was in the intracranial portion after the artery gave its PICA branch (Figures 1,2). No anomaly was detected in other branches of the vertebrobasilary system. The basilar tip aneurysm was treated with endovascular approach (Figure 2).
Figure 1: Preembolization image of the vertebrobasilar system. (LVA: left vertebral artery; RVA: right vertebral artery; BA: basilar artery; BTA: basilar tip aneurysm; PICA: posterior inferior cerebellar artery; AICA: anterior inferior cerebellar artery; SCA: superior cerebellar artery; PCA: posterior cerebral artery)
Intracranial arteries are the sites where aneurysms are most often localized. Many autopsy and angiographic studies showed that the prevalence of intracranial aneurysms in the population is 1-8% [1]. The maximum hemodynamic stress in a vascular plexus is at the bifurcation apex of the vessel. The pressure here is shown to be 2-3 times higher than the maximum pressure within the proximal main artery lumen [3]. Vascular and internal current hemodynamics are of great importance in the occurrence, development and configuration of the intracranial aneurysms [1]. Saccular aneurysms usually develop at the bifurcation points of the arteries proximal to the circle of Willis. The location of these aneurysms is the anterior circulation in 85-90% of the cases, and posterior circulation in 10-15%. In the posterior circulation, there are two common sites: bifurcation point of the basilar artery and the origin of the posterior inferior cerebellar artery (PICA) [1]. The frequency of the aneurysm at the basilar artery bifurcation as reported by Yasargil et al. is 4.9% [4].
The incidence of saccular aneurysm caused by hemodynamic stress increases in cases with congenital anomalies of intracranial vascular structures. Karazincir et al. retrospectively studied the frequency of vascular variations and anomalies accompanying intracranial aneurysms [1]. Only seven (3.1%) basilar tip aneurysms were detected in the angiographs of 190 patients with intracranial aneurysms. Among those, three patients had single aneurysm without any accompanying vascular anomaly. Other four patients had multiple aneurysms and accompanying vascular anomalies (e.g., fetal originated posterior cerebral artery, supraclinoid internal carotid artery aneurysm, fenestration, hypoplasia of the A1 segment of anterior cerebral artery, middle cerebral artery bifurcation). None of these cases had basilar tip aneurysm accompanying a partially hypoplastic left vertebral artery as it is in our case. It is thought that the basilar tip aneurysm in our case was due to the hemodynamic stress in the hypoplastic left VA.
Previous studies gave various results about the diameter of the VA. Yasargil reported the range as 0.92 – 4.09 mm, while in some other radiologic studies it was 3–4 mm [2]. Because of various results in different studies, the definition of VA hypoplasia has not been precisely stated. VAs with less than 2 mm diameter were accepted as hypoplastic in pathoanatomic studies. In ultrasonographic studies, frequency of hypoplastic VA was reported as 1.9% in studies considering a VA diameter less than 2 mm as hypoplastic, and 6% in the cases that have a cut-off value of 3 mm [5].
It is reported that great differences in the diameter of the VAs at a level superior to the first cervical vertebra, play an important role in the etiology of the vertebrobasilar insufficiency [2]. Asymmetry of the intracranial parts of the VAs is common (95%) [6]. It is known that left VA is usually larger than the right one [2,5,6]. In a post-mortem study, the prevalence of larger left VA, larger right VA, and equally sized VAs was given as 42%, 32% and 26%, respectively. In an angiographic study these ratios were as follows: 61%, 33% and 6%. Duplex sonographic studies also reported that the left VA was usually larger than the right one [5]. In the present case, the hypoplasia was on the left VA.
It has been also concluded that VA asymmetry leads to basilar deviation [6]. Deviation is usually detected towards the larger VA, to the opposite side. In our case, the BA was deviated to the left, towards the larger right VA.
Vertebrobasilar system anomalies are usually detected by angiography. In the MR angiographic study of Paksoy et al., congenital morphologic anomaly of distal vertebral artery (CMADVA) were found in 88 out of 768 (11.5%) patients with vertigo and in 4 out of 150 (2.7%) control group subjects. For these 88 patients in the vertigo group, there were no other pathologies that would lead to vertigo; hence the authors concluded that such vascular variations could be related to vertigo and dizziness [2]. They accepted 1 mm as cut-off for hypoplasia and classified CMADVA in 10 subgroups. According to this classification the subjects like the ones in our case were grouped as type II (partial unilateral hypoplastic VA (after PICA division). Seventeen out of 88 patients with CMADVA in vertigo group and the 4 subjects (2.3%) with CMADVA in the asymptomatic control group were in Type II [2]. It is remarkable that the entire asymptomatic control group was in Type II in that serial.
The hemodynamic stress caused by the anomalies of the arterial system may play a role in the etiology of an aneurysm. This case is interesting in terms of being a rare example of basilar aneurysm accompanying to an arterial anomaly.
References
- Karazincir S, Ada E, Sarsilmaz A, Yalcin O, Vidinli B, Sahin E. Frequency of vascular variations and anomalies accompanying intracranial aneurysms. Tani Girisim Radyol. 2004; 10: 103–109. (Turkish).
- Paksoy Y, Vatansev H, Seker M, Ustun ME, Buyukmumcu M, Akpinar Z. Congenital morphological abnormalities of the distal vertebral arteries (CMADVA) and their relationship with vertigo and dizziness. Med Sci Monit. 2004; 10: CR316–323.
- Foutrakis GN, Yonas H, Sclabassi RJ. Saccular aneurysm formation in curved and bifurcating arteries. AJNR Am J Neuroradiol. 1999; 20: 1309–1317.
- Lang J. Skull base and related structures. Atlas of clinical anatomy. Stuttgart, Schattauer. 1995; 39.
- Jeng JS, Yip PK. Evaluation of vertebral artery hypoplasia and asymetry by color-coded duplex ultrasonography. Ultrasound Med Biol. 2004; 30: 605–609.
- Kazui S, Kuriyama Y, Naritomi H, Sawada T, Ogawa M, Maruyama M. Estimation of vertebral arterial asymmetry by computed tomography. Neuroradiology. 1989; 31: 237–239.
Deniz Uzmansel1*, Zeliha Kurtoglu1, Celal Bagdatoglu2, Alev Kara1 and Altan Yildiz3
1Mersin University, Faculty of Medicine, Departments of Anatomy,33169, Mersin, Turkey.
2Mersin University, Faculty of Medicine, Departments of Neurosurgery,33169, Mersin, Turkey.
3Mersin University, Faculty of Medicine, Departments ofNeurosurgery and Radiodiagnostic,33169, Mersin, Turkey.
- *Corresponding Author:
- Deniz Uzmansel, MD
Mersin University, Faculty of Medicine Department of Anatomy, Yenisehir Campus Mersin, 33169,Turkey.
Tel: +90 (324) 3412815/1053
E-mail: duzmansel@yahoo.com
Date of Received: April 9th, 2009
Date of Accepted: August 12th, 2009
Published Online: August 30th, 2009
© IJAV. 2009; 2: 96–98.
Abstract
In a 45-year-old male patient, a congenital anomaly of the intracranial part of the left vertebral artery accompanying an aneurysm of the vertebro-basilar system was encountered. The patient consulted to a neurosurgeon about headache and vertigo, and a cranial CT revealed an aneurysm at the prepontine cistern. In the cerebral angiography, hypoplastic left vertebral artery accompanying an aneurysm of the basilar tip was detected. The left vertebral artery gave off the posterior inferior cerebellar artery, then became hypoplastic and joined with its counterpart to form the basilar artery. This pattern is called as type II. The aneurysm of the basilar tip was cured via endovascular route. The congenital anomaly discussed on its association with vertigo and aneurysm of basilar tip.
-Keywords
basilar artery,aneurysm,vertebral artery,hypoplasia,vertigo
Introduction
Intracranial aneurysms are classified in 3 groups as saccular (berry), fusiform and dissecting aneurysms, regarding their pathological appearance. Among those, saccular ones constitute 90-95% of all cases, and are found at the bifurcation site where the hemodynamic stress is highest [1].
Arterial anatomy of the posterior cranial fossa is variable. It has been already reported that unequal diameters of the vertebral arteries (VA) cause insufficiency in the vertebrobasilary circulation, which in turn results in vertebrobasilary ischemia [2].
Here, the relation between the basilar tip aneurysm and hypoplastic left vertebral artery, as well as the role of the hypoplasia in vertebrobasilar insufficiency etiology are discussed.
Case Report
A 45-year-old male patient consulted to a neurosurgeon with headache and vertigo, and a cranial CT revealed an aneurysm at the prepontine cistern. A further cerebral angiography showed the aneurysm at the basilar tip where it divides into two posterior cerebral arteries. A partially hypoplastic left VA was also detected. Basilar artery (BA) was formed by the union of a normal right VA and a partially hypoplastic left VA at the bulbopontine junction, and its diameter was 4 mm. The dimension of the basilar tip aneurysm was 12x13 mm. The lumen diameter of the right VA was 3 mm, the left VA was 1.2 mm and 0.8 mm before and after giving the posterior inferior cerebellar artery (PICA), respectively. The BA was deviated to the hypoplastic side. The hypoplastic part of the left VA was in the intracranial portion after the artery gave its PICA branch (Figures 1,2). No anomaly was detected in other branches of the vertebrobasilary system. The basilar tip aneurysm was treated with endovascular approach (Figure 2).
Figure 1: Preembolization image of the vertebrobasilar system. (LVA: left vertebral artery; RVA: right vertebral artery; BA: basilar artery; BTA: basilar tip aneurysm; PICA: posterior inferior cerebellar artery; AICA: anterior inferior cerebellar artery; SCA: superior cerebellar artery; PCA: posterior cerebral artery)
Intracranial arteries are the sites where aneurysms are most often localized. Many autopsy and angiographic studies showed that the prevalence of intracranial aneurysms in the population is 1-8% [1]. The maximum hemodynamic stress in a vascular plexus is at the bifurcation apex of the vessel. The pressure here is shown to be 2-3 times higher than the maximum pressure within the proximal main artery lumen [3]. Vascular and internal current hemodynamics are of great importance in the occurrence, development and configuration of the intracranial aneurysms [1]. Saccular aneurysms usually develop at the bifurcation points of the arteries proximal to the circle of Willis. The location of these aneurysms is the anterior circulation in 85-90% of the cases, and posterior circulation in 10-15%. In the posterior circulation, there are two common sites: bifurcation point of the basilar artery and the origin of the posterior inferior cerebellar artery (PICA) [1]. The frequency of the aneurysm at the basilar artery bifurcation as reported by Yasargil et al. is 4.9% [4].
The incidence of saccular aneurysm caused by hemodynamic stress increases in cases with congenital anomalies of intracranial vascular structures. Karazincir et al. retrospectively studied the frequency of vascular variations and anomalies accompanying intracranial aneurysms [1]. Only seven (3.1%) basilar tip aneurysms were detected in the angiographs of 190 patients with intracranial aneurysms. Among those, three patients had single aneurysm without any accompanying vascular anomaly. Other four patients had multiple aneurysms and accompanying vascular anomalies (e.g., fetal originated posterior cerebral artery, supraclinoid internal carotid artery aneurysm, fenestration, hypoplasia of the A1 segment of anterior cerebral artery, middle cerebral artery bifurcation). None of these cases had basilar tip aneurysm accompanying a partially hypoplastic left vertebral artery as it is in our case. It is thought that the basilar tip aneurysm in our case was due to the hemodynamic stress in the hypoplastic left VA.
Previous studies gave various results about the diameter of the VA. Yasargil reported the range as 0.92 – 4.09 mm, while in some other radiologic studies it was 3–4 mm [2]. Because of various results in different studies, the definition of VA hypoplasia has not been precisely stated. VAs with less than 2 mm diameter were accepted as hypoplastic in pathoanatomic studies. In ultrasonographic studies, frequency of hypoplastic VA was reported as 1.9% in studies considering a VA diameter less than 2 mm as hypoplastic, and 6% in the cases that have a cut-off value of 3 mm [5].
It is reported that great differences in the diameter of the VAs at a level superior to the first cervical vertebra, play an important role in the etiology of the vertebrobasilar insufficiency [2]. Asymmetry of the intracranial parts of the VAs is common (95%) [6]. It is known that left VA is usually larger than the right one [2,5,6]. In a post-mortem study, the prevalence of larger left VA, larger right VA, and equally sized VAs was given as 42%, 32% and 26%, respectively. In an angiographic study these ratios were as follows: 61%, 33% and 6%. Duplex sonographic studies also reported that the left VA was usually larger than the right one [5]. In the present case, the hypoplasia was on the left VA.
It has been also concluded that VA asymmetry leads to basilar deviation [6]. Deviation is usually detected towards the larger VA, to the opposite side. In our case, the BA was deviated to the left, towards the larger right VA.
Vertebrobasilar system anomalies are usually detected by angiography. In the MR angiographic study of Paksoy et al., congenital morphologic anomaly of distal vertebral artery (CMADVA) were found in 88 out of 768 (11.5%) patients with vertigo and in 4 out of 150 (2.7%) control group subjects. For these 88 patients in the vertigo group, there were no other pathologies that would lead to vertigo; hence the authors concluded that such vascular variations could be related to vertigo and dizziness [2]. They accepted 1 mm as cut-off for hypoplasia and classified CMADVA in 10 subgroups. According to this classification the subjects like the ones in our case were grouped as type II (partial unilateral hypoplastic VA (after PICA division). Seventeen out of 88 patients with CMADVA in vertigo group and the 4 subjects (2.3%) with CMADVA in the asymptomatic control group were in Type II [2]. It is remarkable that the entire asymptomatic control group was in Type II in that serial.
The hemodynamic stress caused by the anomalies of the arterial system may play a role in the etiology of an aneurysm. This case is interesting in terms of being a rare example of basilar aneurysm accompanying to an arterial anomaly.
References
- Karazincir S, Ada E, Sarsilmaz A, Yalcin O, Vidinli B, Sahin E. Frequency of vascular variations and anomalies accompanying intracranial aneurysms. Tani Girisim Radyol. 2004; 10: 103–109. (Turkish).
- Paksoy Y, Vatansev H, Seker M, Ustun ME, Buyukmumcu M, Akpinar Z. Congenital morphological abnormalities of the distal vertebral arteries (CMADVA) and their relationship with vertigo and dizziness. Med Sci Monit. 2004; 10: CR316–323.
- Foutrakis GN, Yonas H, Sclabassi RJ. Saccular aneurysm formation in curved and bifurcating arteries. AJNR Am J Neuroradiol. 1999; 20: 1309–1317.
- Lang J. Skull base and related structures. Atlas of clinical anatomy. Stuttgart, Schattauer. 1995; 39.
- Jeng JS, Yip PK. Evaluation of vertebral artery hypoplasia and asymetry by color-coded duplex ultrasonography. Ultrasound Med Biol. 2004; 30: 605–609.
- Kazui S, Kuriyama Y, Naritomi H, Sawada T, Ogawa M, Maruyama M. Estimation of vertebral arterial asymmetry by computed tomography. Neuroradiology. 1989; 31: 237–239.