Unique case of a replaced right hepatic artery
Katherine E Kondratuk*, Elizabeth Laskowski, Stuart Inglis
School of Medicine and Biomedical Sciences, Pathology and Anatomical Sciences, USA.
- *Corresponding Author:
- Kondratuk KE
Department of Pathology and Anatomical Sciences
University at Buffalo, School of Medicine and Biomedical Sciences Pathology and Anatomical Sciences, USA
Telephone 1 (716) 524-0236
E-mail: stuartin@buffalo.edu
Published Online: 2 June 2017
Citation : Kondratuk KE, Laskowski K, Inglis S. Unique case of a replaced right hepatic artery. Int J Anat Var. 2017;10(2):014-15.
© This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http:// creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
[ft_below_content] =>Keywords
Liver, Hepatic artery, Pancreaticoduodenal artery, Vasculature, Gastrointestinal
Introduction
Agreat deal of variability exists in the vascular supply to the liver. The traditional view of a proper hepatic artery branching from the common hepatic artery and giving rise to the left and right hepatic arteries may occur in only 55% of the population [1]. In 10-20% of the population, a right hepatic artery (RHA) may instead originate from the superior mesenteric artery (SMA) [2]. This may exist as an accessory branch secondary to a RHA originating from the common hepatic artery, or as a replaced branch providing the exclusive blood supply to the right liver lobe [3]. Presence of an accessory or replaced RHA (A/R RHA) can complicate surgeries, interventional radiology procedures and organ transplantations. This can be further complicated with the additional variation of the inferior pancreaticoduodenal artery (IPDA) sharing a common origin with the A/R RHA [4].
Case report
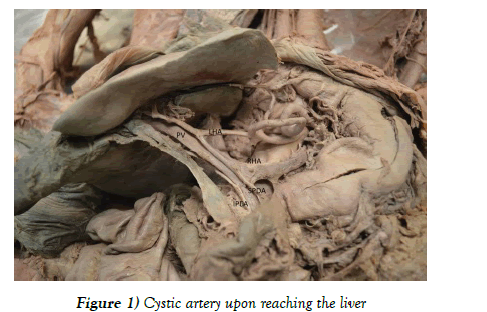
Routine dissection of an 87-year old Caucasian female cadaver revealed a replaced right hepatic artery (RRHA), which originated from the SMA and coursed posterior to the portal vein and gave rise to the cystic artery upon reaching the liver (Figure 1).
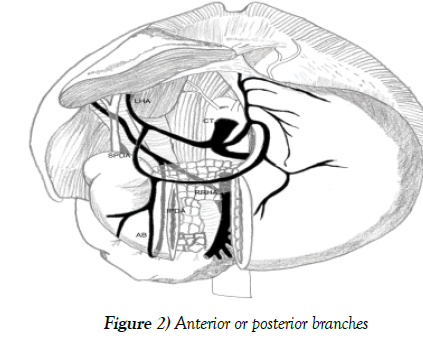
The IPDA shared a common origin with the RRHA and measured 6.1 cm from the point of origin. After originating with the RRHA the IPDA traveled inferiorly to reach the posterior head of the pancreas. At the superior border of the posterior pancreatic head, the IPDA gave off an anastomosing branch that joined with the superior pancreaticoduodenal artery (SPDA) before the SPDA split into anterior and posterior branches. The IPDA did not give off anterior or posterior branches (Figure 2).
Discussion
Variations in hepatic vasculature are common with the accepted standard anatomy accounting for only 55% of the population [1]. These variants were classified into ten types by Michels based on dissection of 200 cadavers [1]. The present case of an A/R RHA can be classified as Type 3 according to Michels’ scheme and is observed in 10-20% of the population [5-8]. In this case the RRHA also shares a common origin with the IPDA. Peripancreatic vasculature displays great variation and the vasculature of the pancreatic head is especially complex [9]. The IPDA in particular is a major source of variation [10]. The combined variation of a RRHA sharing a common origin with the IPDA is uncommon with angiographic studies showing a prevalence of less than 3% [3,4,9].
Variations of this abdominal vasculature arise during embryological development. Four vitelline arteries connected by a longitudinal anterior anastomosis are involved in the development of abdominal vasculature supplying the stomach, spleen, liver, pancreas, and intestines. Abnormal persistence or regression of these embryonic arteries may give rise to an anatomic variant of the celiac trunk or SMA [11].
Presence of an A/R RHA is not typically pathological. One potential pathology is associated with occlusion of the SMA. 4% of all arterial emboli lodge in the SMA. In cases where an A/R RHA is present, the liver may also become necrotic. No reports have suggested pathology related to the IPDA sharing a common origin with a RRHA. Considering the age at death, lack of GI pathology, and cause of death of this individual, it seems unlikely that this specific variant caused any medical complications.
Hepatic artery variations have dangerous clinical implications, especially in cases where the variation is a RRHA. Aberrant RHAs (aRHAs) are the most frequently encountered vascular anomaly during pancreaticoduodenectomy procedures [12]. The presence of an aRHA has been associated with increased pancreaticoduodenectomy operative time and blood loss, although the differences were not significant [2]. The presence of an aRHA also complicates the procedure as these variant arteries are most susceptible to intraoperative damage and tumor involvement [12]. In order to avoid complications during surgical procedures the RRHA should be identified before the procedure to minimize the risk of vascular damage [13]. It is also important to know the distribution of peripancreatic vasculature prior to transarterial interventions, such as infusion of protease inhibitor for acute pancreatitis and infusion chemotherapy for pancreatic carcinoma [9].
Aberrant hepatic vasculature poses a unique challenge in transplantation procedures. As aberrant vasculature supplies a distinct area of the liver, transplantation in the case of a RRHA requires back-bench reconstruction [4]. Though studies have suggested a RRHA is beneficial in cases of right liver living donors [13], the situation is complicated when multiple organs are transplanted and peripancreatic vascular variations are present. When the IPDA shares a common origin with the A/RRHA, multi-organ transplantation becomes especially difficult. Distribution of the IPDA to the liver team with the A/RRHA without IPDA reconstruction would likely result in ischemia of the pancreatic head. Several approaches to multi-organ transplantation in this setting have been previously described. One method uses the splenic artery to supply blood to the A/R RHA and the entire SMA is used for the pancreatic allograft [14,15]. Due to the drawbacks of this method, such as time-intensive dissection of the A/R RHA and the potential for a 90-degree twist of the A/R RHA, Huang et al. proposed an alternative method. They suggest the gastroduodenal artery be used to supply blood to the A/R RHA. This is proposed as a superior method due to the similar diameters of the two arteries, and this method preserves the IPDA for the pancreatic allograft [4].
Acknowledgements
The authors wish to thank all individuals who donate their bodies and tissues for the advancement of education and research.
The authors wish to acknowledge Dr. Henry Vandyke Carter (1831- 1897), whose classical anatomical illustrations served as inspiration for the schematic representation used in the present paper.
References
- Michels NA. Newer anatomy of the liver and its variant blood supply and collateral circulation. Am J Surg. 1966;112:337-47.
- Rebibo L, Peltier J, Gerin O, et al. Unusual course of the aberrant right hepatic artery running through the pancreatic parenchyma during modified Frey’s procedure. Morphologie. 2014;98:182-6.
- Cherian PT, Hegab B, Oliff SP, et al. The management of an accessory or replaced right hepatic artery during multiorgan retrieval: results of an angiographic study. Liver Transpl. 2010;16:742-7.
- Huang Y, Li J, Qi H. Management of the accessory or replaced right hepatic artery (A/R RHA) during multiorgan retrieval when the inferior pancreaticoduodenal artery shares a common origin with A/R RHA. Transplant Proc. 2013;45:20-4.
- Abdullah SS, Mabrut JY, Garbit V, et al. Anatomical variations of the hepatic artery: study of 932 cases in liver transplantation. Surg Radiol Anat. 2006;28:468-73.
- Saba L, Mallarini G. Anatomical variations of arterial liver vascularization: an analysis by using MDCTA. Surg Radiol Anat. 2011;33:559-68.
- Sebben GA, Rocha SL, Sebben MA, et al. Variations of hepatic artery: anatomical study on cadavers. Rev Col Bras Cir. 2012;40:221-6.
- Dandekar U, Dandekar K, Chavan S. Right hepatic artery: a cadaver investigation and its clinical significance. Anat Res Int. 2015;412595.
- Okahara M, Mori H, Kiyosue H, et al. Arterial supply to the pancreas; variations and cross-sectional anatomy. Abdom Imaging. 2010;35:134-42.
- Bertelli E, Gregorio FD, Bertelli L, et al. The arterial blood supply of the pancreas: a review III. The inferior pancreaticoduodenal artery. An anatomical review and a radiological study. Surg Radiol Anat. 1996;18:67-74.
- Kalthur SG, Sarda R, Bankar M. Multiple vascular variations of abdominal vessels in a male cadaver: embryological perspective and clinical importance. J Morphol Sci. 2011;28:152-6.
- Rammohan A, Palaniappan R, Pitchaimuthu A, et al. Implications of the presence of an aberrant right hepatic artery in patients undergoing pancreaticoduodenectomy. World J Gastrointest Surg. 2014;6:9-13.
- Moon JJ, Wijdicks CA, Williams JM. Right hepatic artery branching off the superior mesenteric artery and its potential implications. Int J Anat Var. 2009;2:143-5.
- Colledan M, Ferla G, Rossi G, et al. Bench reconstruction of the graft arterial supply in liver transplantation. Transplant Proc. 1990;22:408-9.
- Shaw BW, Iwatsuki S, Starzl TE. Alternative methods of arterialization of the hepatic graft. Surg Gynecol Obstet. 1984;159:490-3.
Katherine E Kondratuk*, Elizabeth Laskowski, Stuart Inglis
School of Medicine and Biomedical Sciences, Pathology and Anatomical Sciences, USA.
- *Corresponding Author:
- Kondratuk KE
Department of Pathology and Anatomical Sciences
University at Buffalo, School of Medicine and Biomedical Sciences Pathology and Anatomical Sciences, USA
Telephone 1 (716) 524-0236
E-mail: stuartin@buffalo.edu
Published Online: 2 June 2017
Citation : Kondratuk KE, Laskowski K, Inglis S. Unique case of a replaced right hepatic artery. Int J Anat Var. 2017;10(2):014-15.
© This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http:// creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The case of a replaced right hepatic artery sharing a common origin with the inferior pancreaticoduodenal artery is reported. A right hepatic artery originating from the superior mesenteric artery occurs in 10-20% of the population. When a right hepatic artery is replaced and shares a common origin with the inferior pancreaticoduodenal artery the combined variation has a prevalence of <3%. This variant is not typically associated with pathology except in cases of superior mesenteric artery occlusion. A replaced right hepatic artery may have dangerous clinical consequences if the variant is not recognized before pancreaticoduodenectomy and laproscopic cholecystectomy procedures. The distribution of peripancreatic vasculature should be discerned prior to transarterial interventions. Specific details of the observed case are reported and the clinical and surgical considerations are further discussed.
-Keywords
Liver, Hepatic artery, Pancreaticoduodenal artery, Vasculature, Gastrointestinal
Introduction
Agreat deal of variability exists in the vascular supply to the liver. The traditional view of a proper hepatic artery branching from the common hepatic artery and giving rise to the left and right hepatic arteries may occur in only 55% of the population [1]. In 10-20% of the population, a right hepatic artery (RHA) may instead originate from the superior mesenteric artery (SMA) [2]. This may exist as an accessory branch secondary to a RHA originating from the common hepatic artery, or as a replaced branch providing the exclusive blood supply to the right liver lobe [3]. Presence of an accessory or replaced RHA (A/R RHA) can complicate surgeries, interventional radiology procedures and organ transplantations. This can be further complicated with the additional variation of the inferior pancreaticoduodenal artery (IPDA) sharing a common origin with the A/R RHA [4].
Case report
Routine dissection of an 87-year old Caucasian female cadaver revealed a replaced right hepatic artery (RRHA), which originated from the SMA and coursed posterior to the portal vein and gave rise to the cystic artery upon reaching the liver (Figure 1).
The IPDA shared a common origin with the RRHA and measured 6.1 cm from the point of origin. After originating with the RRHA the IPDA traveled inferiorly to reach the posterior head of the pancreas. At the superior border of the posterior pancreatic head, the IPDA gave off an anastomosing branch that joined with the superior pancreaticoduodenal artery (SPDA) before the SPDA split into anterior and posterior branches. The IPDA did not give off anterior or posterior branches (Figure 2).
Discussion
Variations in hepatic vasculature are common with the accepted standard anatomy accounting for only 55% of the population [1]. These variants were classified into ten types by Michels based on dissection of 200 cadavers [1]. The present case of an A/R RHA can be classified as Type 3 according to Michels’ scheme and is observed in 10-20% of the population [5-8]. In this case the RRHA also shares a common origin with the IPDA. Peripancreatic vasculature displays great variation and the vasculature of the pancreatic head is especially complex [9]. The IPDA in particular is a major source of variation [10]. The combined variation of a RRHA sharing a common origin with the IPDA is uncommon with angiographic studies showing a prevalence of less than 3% [3,4,9].
Variations of this abdominal vasculature arise during embryological development. Four vitelline arteries connected by a longitudinal anterior anastomosis are involved in the development of abdominal vasculature supplying the stomach, spleen, liver, pancreas, and intestines. Abnormal persistence or regression of these embryonic arteries may give rise to an anatomic variant of the celiac trunk or SMA [11].
Presence of an A/R RHA is not typically pathological. One potential pathology is associated with occlusion of the SMA. 4% of all arterial emboli lodge in the SMA. In cases where an A/R RHA is present, the liver may also become necrotic. No reports have suggested pathology related to the IPDA sharing a common origin with a RRHA. Considering the age at death, lack of GI pathology, and cause of death of this individual, it seems unlikely that this specific variant caused any medical complications.
Hepatic artery variations have dangerous clinical implications, especially in cases where the variation is a RRHA. Aberrant RHAs (aRHAs) are the most frequently encountered vascular anomaly during pancreaticoduodenectomy procedures [12]. The presence of an aRHA has been associated with increased pancreaticoduodenectomy operative time and blood loss, although the differences were not significant [2]. The presence of an aRHA also complicates the procedure as these variant arteries are most susceptible to intraoperative damage and tumor involvement [12]. In order to avoid complications during surgical procedures the RRHA should be identified before the procedure to minimize the risk of vascular damage [13]. It is also important to know the distribution of peripancreatic vasculature prior to transarterial interventions, such as infusion of protease inhibitor for acute pancreatitis and infusion chemotherapy for pancreatic carcinoma [9].
Aberrant hepatic vasculature poses a unique challenge in transplantation procedures. As aberrant vasculature supplies a distinct area of the liver, transplantation in the case of a RRHA requires back-bench reconstruction [4]. Though studies have suggested a RRHA is beneficial in cases of right liver living donors [13], the situation is complicated when multiple organs are transplanted and peripancreatic vascular variations are present. When the IPDA shares a common origin with the A/RRHA, multi-organ transplantation becomes especially difficult. Distribution of the IPDA to the liver team with the A/RRHA without IPDA reconstruction would likely result in ischemia of the pancreatic head. Several approaches to multi-organ transplantation in this setting have been previously described. One method uses the splenic artery to supply blood to the A/R RHA and the entire SMA is used for the pancreatic allograft [14,15]. Due to the drawbacks of this method, such as time-intensive dissection of the A/R RHA and the potential for a 90-degree twist of the A/R RHA, Huang et al. proposed an alternative method. They suggest the gastroduodenal artery be used to supply blood to the A/R RHA. This is proposed as a superior method due to the similar diameters of the two arteries, and this method preserves the IPDA for the pancreatic allograft [4].
Acknowledgements
The authors wish to thank all individuals who donate their bodies and tissues for the advancement of education and research.
The authors wish to acknowledge Dr. Henry Vandyke Carter (1831- 1897), whose classical anatomical illustrations served as inspiration for the schematic representation used in the present paper.
References
- Michels NA. Newer anatomy of the liver and its variant blood supply and collateral circulation. Am J Surg. 1966;112:337-47.
- Rebibo L, Peltier J, Gerin O, et al. Unusual course of the aberrant right hepatic artery running through the pancreatic parenchyma during modified Frey’s procedure. Morphologie. 2014;98:182-6.
- Cherian PT, Hegab B, Oliff SP, et al. The management of an accessory or replaced right hepatic artery during multiorgan retrieval: results of an angiographic study. Liver Transpl. 2010;16:742-7.
- Huang Y, Li J, Qi H. Management of the accessory or replaced right hepatic artery (A/R RHA) during multiorgan retrieval when the inferior pancreaticoduodenal artery shares a common origin with A/R RHA. Transplant Proc. 2013;45:20-4.
- Abdullah SS, Mabrut JY, Garbit V, et al. Anatomical variations of the hepatic artery: study of 932 cases in liver transplantation. Surg Radiol Anat. 2006;28:468-73.
- Saba L, Mallarini G. Anatomical variations of arterial liver vascularization: an analysis by using MDCTA. Surg Radiol Anat. 2011;33:559-68.
- Sebben GA, Rocha SL, Sebben MA, et al. Variations of hepatic artery: anatomical study on cadavers. Rev Col Bras Cir. 2012;40:221-6.
- Dandekar U, Dandekar K, Chavan S. Right hepatic artery: a cadaver investigation and its clinical significance. Anat Res Int. 2015;412595.
- Okahara M, Mori H, Kiyosue H, et al. Arterial supply to the pancreas; variations and cross-sectional anatomy. Abdom Imaging. 2010;35:134-42.
- Bertelli E, Gregorio FD, Bertelli L, et al. The arterial blood supply of the pancreas: a review III. The inferior pancreaticoduodenal artery. An anatomical review and a radiological study. Surg Radiol Anat. 1996;18:67-74.
- Kalthur SG, Sarda R, Bankar M. Multiple vascular variations of abdominal vessels in a male cadaver: embryological perspective and clinical importance. J Morphol Sci. 2011;28:152-6.
- Rammohan A, Palaniappan R, Pitchaimuthu A, et al. Implications of the presence of an aberrant right hepatic artery in patients undergoing pancreaticoduodenectomy. World J Gastrointest Surg. 2014;6:9-13.
- Moon JJ, Wijdicks CA, Williams JM. Right hepatic artery branching off the superior mesenteric artery and its potential implications. Int J Anat Var. 2009;2:143-5.
- Colledan M, Ferla G, Rossi G, et al. Bench reconstruction of the graft arterial supply in liver transplantation. Transplant Proc. 1990;22:408-9.
- Shaw BW, Iwatsuki S, Starzl TE. Alternative methods of arterialization of the hepatic graft. Surg Gynecol Obstet. 1984;159:490-3.