Unique Case of Aberrant Nerves to Serratus Anterior Muscles with Unusual Branching Pattern of Posterior Cord of Left Brachial Plexus
Received: 27-Jul-2022, Manuscript No. ijav-22-5205; Editor assigned: 29-Jul-2022, Pre QC No. ijav-22-5205 (PQ); Accepted Date: Aug 16, 2022; Reviewed: 12-Aug-2022 QC No. ijav-22-5205; Revised: 16-Aug-2022, Manuscript No. ijav-22-5205 (R); Published: 23-Aug-2022, DOI: 10.37532/1308-4038.15(8).210
Citation: Tessema CB. Unique Case of Aberrant Nerves to Serratus Anterior Muscles with Unusual Branching Pattern of Posterior Cord of Left Brachial Plexus. Int J Anat Var. 2022;15(8):204-206.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
During the dissection of an 81-year-old male cadaver, interconnected nerve trunks from C6 and C7 to the serratus anterior muscles were revealed bilaterally. These trunks broke up into divisions that gave multiple branches to the muscle; the most inferior of the branches followed the course of long thoracic nerve. In the left axilla, the posterior cord of the brachial plexus gave multiple branches innervating the subscapularis, latissimus dorsi, teres major and teres minor muscles. With exception of the two upper subscapular nerves that originated directly from the posterior cord, the rest arose indirectly from axillary nerve independently and via a common stem. Such variable nerves that occur in multiples carry a potential risk of nerve injury during clinical procedure, which requires awareness and attention to avoid unintended complications as well as to advert their potential use in the treatment of other nerve injuries.
Keywords
Nerves to serratus anterior; Posterior cord of brachial plexus, Axillary nerve; Subscapular nerves; Thoracodorsal nerve
INTRODUCTION
The serratus anterior muscle (SAM) is innervated by the long thoracic nerve (LTN) formed by fibers from C5, C6 and C7 roots of the brachial plexus (BP), although the C7 may be absent [1]. After obliquely piercing through the middle scalene muscle, the C5 and C6 roots unit within the muscle or lateral to it and may be joined by the C7 root which emerges between the anterior and middle scalene muscles [1]. Then it descends dorsal to the BP and the first segment of the axillary artery and crosses the superior border of SAM to reach its lateral surface [1]. A previous anatomical and functional assessment study of LTN on fifteen cadavers found that it arises from the C5, C6 and C7, where the C5 and C6 were joined beneath the middle scalene muscle to form the upper division. A late reunion with the lower division formed by C7 occurred caudally in the axillary region [2]. Another study done on the right and left sides of 18 cadavers demonstrated the relationship between these three nerve roots and the scalene muscles, where in 61% of the sides C7 joined C5 and C6 to form the LTN, in 56% of the sides it was found between the middle and posterior scalene muscles and in 11% of the sides the C5 and C6 components traveled through the middle scalene muscle and combined with C7, which was always located anterior to the middle scalene muscle. In two of the sides the C5, C6, and C7 contributions to the LTN were located between the middle scalene and the BP without passing through any muscle [3]. Some other studies did document a broader range of variability in the origin of LTN. One of these studies done on 57 cadavers revealed that in 36% of the cases the LTN originated from C5, 6 and 7, while C5 was absent in 6% and C7 was absent in 10% of the cases [4]. Related to its further course, a retrospective study of the thoracic portion of the LTN conducted on 43 patients noted that in 79% of the cases a single major nerve coursing along the SAM classified as type I LTN was observed, while in about 21% of the cases two equal sized major branches of the nerve were identified and classified as type II LTN [5]. The unique course of the LTN through the interscalene triangle, middle scalene muscle and its superficial descent along the mid axillary line to the SAM predisposes it to injury caused by various factors leading to winged scapula. This injury often results from closed trauma leading to compression, stretching or traction of the nerve by direct extrinsic forces or by penetrating injury or by neuritis such as Parsonage-Turner syndrome [6].
It is well established that three subscapular nerves (upper, middle or thoracodorsal and lower) arise from the posterior cord of the BP. The upper subscapular nerve innervates the upper fibers of subscapularis muscle and the lower scapular nerve innervates the lower fibers of subscapularis and teres major muscle, while the middle subscapular (thoracodorsal) nerve innervated the latissimus dorsi muscle. Though, the subscapularis muscle is innervated by the upper and lower subscapular nerves from the posterior cord of the brachial plexus; it is also known that the axillary nerve gives a significant innervation to its lower fibers (25%) [7-8]. A substantial number of other documentations that demonstrate variation in the origin, number and distribution of subscapular nerves also exist. A previous case report noted that two upper subscapular nerves, one from the suprascapular nerve and the other from the posterior division of the upper trunk of the BP that innervated the upper fibers of the subscapularis muscle [9]. There was also a case report in which the posterior cord of the BP gave branch to only radial and axillary nerves, while the upper subscapular, thoracodorsal and lower subscapular nerves were branches from the axillary nerve [10]. As stated in a study done on forty specimens, the thoracodorsal nerve originated from the posterior cord of BP in 72.5%, from the axillary nerve in 15% and arose from the posterior cord of BP by a common stem with the axillary nerve in 12.5% of the case [11]. Another dissection study done by Bhoshale and his coworker on 20 cadavers revealed that the lower subscapular nerve originated from the axillary nerve in 57.5%, from the posterior cord of BP in 37.5% and from a common trunk with axillary nerve in 5% of the cases [12].
All these documentations demonstrate that there is an extensive variation in the origin, number and distribution patterns of nerves to SAM and branches of the posterior cord of the BP in the lateral neck and axillary regions, which are common site for various anesthetic, imaging and surgical procedure.
MATERIALS AND METHODS
During the routine dissection of the posterior cervical triangles of 81-yearold male cadaver, two nerve trunks exiting the neck posterior to the trunks of the BPs of both sides were incidentally found. After lateral reflections of the pectoral muscles and removal of the clavicle, these nerve trunks with unusual complex communications, divisions, and distribution patterns were carefully dissected and followed down to the axilla until they entered the SAM. The right BP was detached at its roots and reflected laterally to show the exact origins of these nerves from C6 and C7 roots. Further cleansing of the posterior axillary wall also revealed multiple branches that directly and indirectly originated from the posterior cord of BP. Photographs were taken for illustrations and the nerves entering SAM were then named as “nerves to serratus anterior” instead of long thoracic nerve and the parts of these nerves from roots to the SAM were designated as trunks, divisions and branches for the convenience of description in this particular report.
CASE REPORT
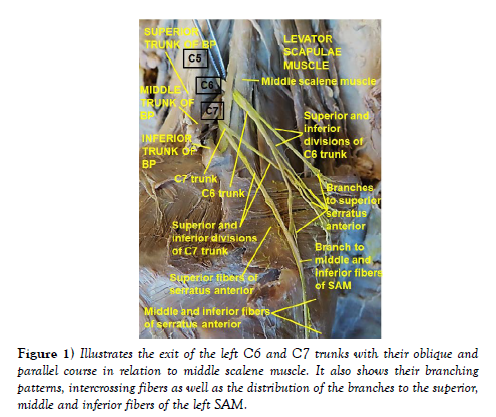
Left side: Two nerve trunks to SAM originated from the dorsal aspects of C6 and C7 roots, exited the neck and descended on the superior aspect of the lateral thoracic wall. The C6 trunk first ran through the interscalene triangle and pierced through the superficial aspect of the middle scalene muscle, while the C7 trunk exited through the interscalene triangle (Figure 1). Then both took an oblique and parallel descent on the lateral surface of the middle scalene muscle where the two trunks uniquely divided into superior and inferior divisions. The inferior division of the C6 trunk re-divided into three branches. The most inferior of these branches descended superficial to the superior fibers of SAM, crossed over the superior division of the C7 trunk, gave two branches to the inferior portion of the superior fibers of SAM and joined the inferior division of C7 trunk to descend along the midaxillary line to enter the middle and inferior fibers of the SAM. The remaining two branches of the inferior division of C6 trunk, the superior divisions of C6 and C7 trunks entered the superior fibers of the SAM (Figure 1).
Figure 1: Illustrates the exit of the left C6 and C7 trunks with their oblique and parallel course in relation to middle scalene muscle. It also shows their branching patterns, intercrossing fibers as well as the distribution of the branches to the superior, middle and inferior fibers of the left SAM.
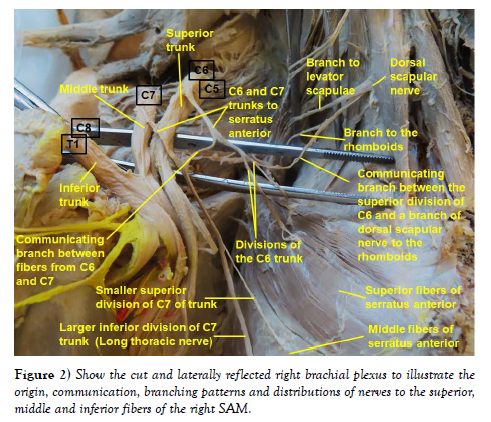
Right side: Similar to the left side, two nerve trunks originated from the dorsal aspects of C6 and C7 roots, but both exited the lateral neck through the interscalene triangle. After exiting through the interscalene triangle the C6 and C7 trunks were interconnected by a communicating branch. Then the post-communicating part of C6 trunk divided into superior and inferior divisions that entered the superior fibers of SAM. The superior division of the C6 trunk was also found to have connection with the branch of dorsal scapular nerve to the rhomboids by another communicating branch. The post-communicating part of the C7 trunk also divided into a smaller superior division and a larger inferior division. The smaller superior division directly entered the middle fibers of SAM, while its larger inferior division descended along the midaxillary line to end on the inferior fibers of SAM (Figure 2).
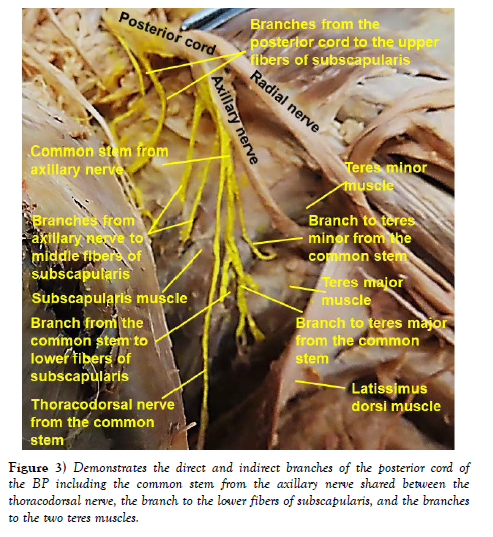
Subscapular nerves on the left side: In the left axilla, in addition to the variant nerves to SAM, multiple branches arising directly from the posterior cord of the BP and indirectly from the axillary nerve to the subscapularis, latissimus dorsi, teres major and teres minor muscles were encountered. Five branches were found to enter the subscapularis muscle. Two of these branches were directly from the posterior cord of the BP to its upper fibers, two were from the axillary nerve to its middle fibers and one branch to its inferior fibers was from a common stem from the axillary nerve shared with the thoracodorsal nerve and the branches to teres major and teres minor muscles (Figure 3).
DISCUSSION
Even though, it is a classic knowledge that the SAM is innervated by the LTN that arises from the C5, C6 and C7 roots with a possible absence of C7 [1]; it is also known that all the three roots consistently contributed to the formation of LTN [2, 3]. Contrary to this notion, there are many other studies and case reports that documented the absence of C5 or C7 roots, more frequently the C7 root of LTN [4]. The formation of the LTN in relation to the middle scalene muscle was also described in such a way that the upper division contributed by C5 and C6 is formed beneath the middle scalene muscle and joined by the lower division from C7 in the axilla [4]. Moreover, it was also stated that this nerve reached the SAM as a single major nerve or as two equal major nerves [5]. However, as observed in this current case report, there was no contribution by C5 and no direct union between C6 and C7 to form distinct major nerves to the SAM, rather different sets of branches from C6 and C7 entered the three parts of the serratus anterior muscles. Nonetheless, the branch formed by the union of the inferior divisions of the left C6 and C7 trunks and the post-communicating part of right C7 trunk followed a similar course to the classic LTN. Therefore, the observation in the current case report is different from these previous documentations for a multitude of peculiar variations in a single cadaver that consisted of the: 1) absence of contribution by C5 on both sides, 2) unusual course of the left C6 through the interscalene triangle and then through the superficial part of the middle scalene muscle, 3) descent of the inferior branch of left C6 to unit with the inferior division of C7 in the axilla to enter the middle and inferior fibers of SAM, 4) slight ascent of the superior division of the left C7 trunk to enter the superior fibers of SAM, 5) connection between the right C6 and C7 trunks by a communicating branch, and 6) communication of the superior division of the right C6 trunk with the branch of dorsal scapular nerve to the rhomboids. The author of this report believes that the peculiar intercross between the branch of the inferior division of the left C6 and superior division of left C7 to reach the inferior and superior fibers of SAM respectively is unique and the 1st of its kind. The unusual interconnection between the right C6 and C7 trunks via a communicating branch, the distribution of C6 branches only to the superior fibers of SAM and its communication with the branch of dorsal scapular nerve makes it completely different from the documentations available so far. Of note are also the distribution of the two branches from the post-communicating part of the right C7 to the middle and inferior fibers of serratus anterior muscle. This kind of course, branching and distribution pattern is also very unique and is not found in any of the reviewed literature.
It is well known that, the unique course of LTN in relation to the middle scalene muscle and its superficial course in the axilla, predisposes it to injury caused by various factors that results in scapular winging [6]. As author of this case report, since there is no formation of LTN in its classic sense, I believe that having innervation by multiple widely distributed branches like this can have advantages and disadvantages as it relates to nerve injuries. On one hand, for it is less likely that all the branches may be encountered at the same time during procedures or trauma, it could decrease the risk of complete loss of function due to isolated nerve injury. On the other hand, the presence of such broad branching pattern could predispose the nerves to inadvertent injury due to difficulty to safe-guard all small branches. Thus, could be associated with a high risk of injury to one or more of these branches leading to partial paralysis or weakness of the muscle.
Even so, it is a well-known fact that the subscapularis muscle is innervated by the upper and lower subscapular nerves from the posterior cord of the BP, it is also innervated by a branch of the axillary nerve [7, 8]. Along with this, a wide range of variations of these nerves is also well documented. These variations included double upper subscapular nerves that separately originated from the posterior cord of the BP and the suprascapular nerve [9], the branches of subscapular nerves including the dorsal scapular nerve arising from the axillary nerve [10], the thoracodorsal nerve originating from the axillary nerve and from the posterior cord of BP by a common stem with the axillary nerve [11, 12]. In contrary to these previous descriptions, the current case report demonstrated that the subscapularis muscle is innervated by five branches, some of which were directly from the posterior cord of BP and the others indirectly from its branch (axillary nerve) that arose independently and by a common stem together with the nerves to the latissimus dorsi and teres muscles. This finding related to the subscapular nerves in this report is completely different from those previously noted findings. Alike the nerves to the SAM, the multiplicity of these nerves has its own advantages and disadvantages with reduced risk of complete paralysis resulting from single nerve injury and difficulty of sparing all the nerves during procedures with a potential risk of partial paralysis or muscle weakness. Generally, such occurrence of nerves in multiples may also be potentially used in neurotization procedures in the vicinity or nerve harvest procedures in nerve graft/repair surgeries for the treatment of injured nerves.
CONCLUSION
The presence of variable and multiple nerves like this in the lateral neck and axillary region, which are common site for various anesthetic, imaging and surgical procedures, carries a high risk of nerve injury of different severity. Therefore, it requires awareness of anesthesiologists, radiologists and surgeons in order to avoid unintended complications during invasive procedures in those regions as well as to advert their potential use as donor nerves for the treatment of other nerve injuries in the vicinity without a significant effect on the muscles they innervate.
ACKNOWLEDGEMENT
I am thankful to the donor and his families for their invaluable donation and consent for education, research and publication. I would also like to express my gratitude to the department of biomedical sciences for the encouragement and uninterrupted support. As always, I am also grateful to Denelle Kees and John Opland for their immense assistance during the dissection of this cadaver in the gross anatomy lab.
REFERENCES
- Standring S. Gray’s anatomy, the anatomical basis of clinical practice, 40th edition, Churchill Livingstone. Elsevier. 2008; 820-823.
- Bertelli JA, Ghizoni MF. Long thoracic nerve: anatomy and functional assessment. J Bone Joint Surg Am. 2005; 87(5):993-8.
- Tubbs RS, Salter EG, Custis JW. Surgical anatomy of cervical and infraclavicular parts of the long thoracic nerve. J Neurosurg. 2006; 104(5):792- 795.
- Ballesteros LE, Ramirez LM. Variations of the origin of collateral branches emerging from the posterior aspect of the brachial plexus. J Brachial Plex Peripher Nerve Inj. 2007; 23; 2:14.
- Ormsby NM, Hawkes DH, Ng CY. Variation of surgical anatomy of the thoracic portion of the long thoracic nerve. Clin Anat 2022; 3594: 442-446.
- Nath RK, Lyons AB, Bietz G. Microneurolysis and decompression of long thoracic nerve injury are effective in reversing scapular winging: Long-term results in 50 cases. BMC Musculoskelet Disord. 2007; 7(8):25.
- Kasper JC, Itamura JM, Tibone JE, Levin SL et al. Human cadaveric study of subscapularis muscle innervation and guidelines to prevent denervation. J Shoulder Elbow Surg. 2008; 17(4):659-62.
- Kellan P, Khan T, Tashjian RZ. Anatomy of the subscapularis: A review. J Shoulder Elbow Surg. 2019; 3:1-6.
- Paraskevas G, Koutsouflianiotis K, Iliou K, Bitsis T et al. Unusual Origin of a Double Upper Subscapular Nerve from the Suprascapular Nerve and the Posterior Division of the Upper Trunk of the Brachial Plexus: A Case Report. J Clin Diagn Res. 2016; 10(6):01-02.
- Dursun A, Bilkay C, Albay S. A rare variation in the branching pattern of the posterior cord. Int J Anat Var. 2016; 9:29-31.
- Bhosale SM, Mallashetty NS. Study of variations in the branching pattern of thoracodorsal nerve. Int J Res Med Sci. 2014; 2(4):1329-1333.
- Bhoshale SM, Havaldar PP. A study of variations in the branching pattern of lower subscapular nerve. J Clin Diagn Res. 2014; 8(11):AC05-AC07.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref