Unusual course of the vagus nerve in the neck passing anterior to the common carotid artery
Received: 21-Jun-2020 Accepted Date: Aug 19, 2020; Published: 26-Aug-2020, DOI: 10.37532/1308-4038.20.13.15
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Along its cervical part, the vagus nerve can be identified within the carotid sheath, usually in a position posterolateral to the artery and posteromedial to the vein. Herewith, we report a dissection case of a variant left vagus nerve, passing anterior to the common carotid artery. At the level of hyoid bone, the vagus nerve emerged from the space between the internal and external carotid arteries and the internal jugular vein. Then the nerve spiraled on the lateral surface of the common carotid artery and took an anterior position to the vessel. Such anterior course of the vagus nerve to the carotid artery is reported in the literature with varying incidence from 0.7% to 5% at ultrasonographic studies or during surgery. This variant course can be explained as an imperfect posterior shifting during embryonic development. When present this aberrant position of the vagus might hamper surgical neck dissection.
Keywords
Vagus nerve; Variation; Carotid triangle; Neck dissection; Human
Introduction
Along its cervical part, the vagus nerve, the tenth of the cranial nerves, can be identified within the carotid sheath between the internal and common carotid arteries and internal jugular vein [1]. In a more detailed way, the nerve is described as located posterior to the vessels in a position posterolateral to the artery and posteromedial to the vein [2]. This configuration is quite stable and variations are rare [3]. When present, however, the aberrant position of the vagus might hamper surgical neck dissection [4,5].
Case Report
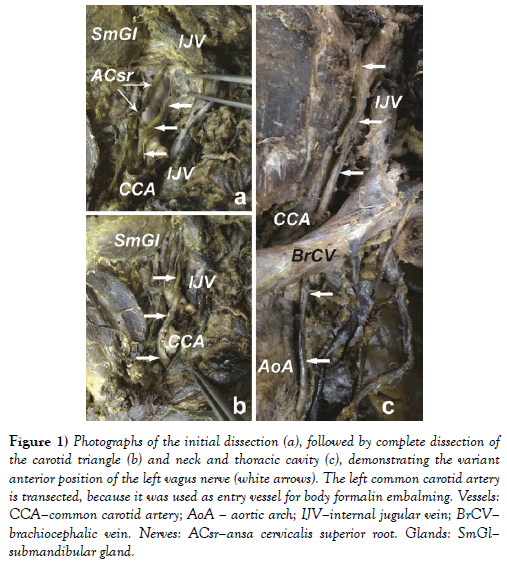
During routine anatomical dissection of the anterior neck region of a 70-yearold Caucasian male cadaver, we discovered a rare variation in the cervical part of the vagus nerve on the left side. After removing the skin and retracting the platysma layer we started a dissection in the left carotid triangle. By retracting the sternocleidomastoid laterally, we exposed the carotid sheath, enveloping the major neurovascular bundle in the region. While dissecting the vessels, we found two parallel nerves emerging from the space between the carotid arteries and internal jugular vein (Figure 1). The smaller anterior nerve was identified as the superior root of ansa cervicalis (Figure 1). It was traced up to the hypoglossal nerve and down to the connection with the inferior root from the cervical plexus. Further dissection identified the larger posterior nerve as a vagus nerve with aberrant course (Figure 1). At the level of the greater horn of hyoid bone, the vagus nerve passed in between the internal and external carotid arteries (medially), and the internal jugular vein (laterally). Then the nerve spiraled on the lateral surface of the common carotid artery and took anterior position to this vessel. After completing the dissection in the lower part of the neck and thorax (Figure 1), we observed a position of the vagus nerve anteriorly in the groove between the common carotid artery and internal jugular vein continuously to the thoracic inlet. Here, the nerve passed between the left common carotid artery and brachiocephalic vein to continue in a common way through the thoracic cavity. No variations in the position and course of the right vagus nerve were observed.
Figure 1: Photographs of the initial dissection (a), followed by complete dissection of the carotid triangle (b) and neck and thoracic cavity (c), demonstrating the variant anterior position of the left vagus nerve (white arrows). The left common carotid artery is transected, because it was used as entry vessel for body formalin embalming. Vessels: CCA–common carotid artery; AoA – aortic arch; IJV–internal jugular vein; BrCV–brachiocephalic vein. Nerves: ACsr–ansa cervicalis superior root. Glands: SmGl–submandibular gland.
Discussion
A course of the vagus nerve anterior to the carotid artery is reported in the literature with varying incidence from 0.7% to 5% [3,6-8]. On ultrasonographic examination of the neck of patients with suspected neck diseases Giovagnorio and Martinoli [7] reported this variation in 0.7% and only on the left side. In another sonographic study, anterior vagus course was observed in 4.3% of the cases, with ratio right to left side - 4:10 [3]. According to AbuRahma and Choueiri [6] anterior vagus course during carotid endarterectomy can be found in less than 5% of the patients. Also, by operative neuromonitoring of the inferior laryngeal nerve during thyroidectomies, anterior course of the vagus nerve was established in 4% [8]. There are cadaveric case reports of this variation on the left side [9] and only one reported case of bilateral anterior course of the vagus nerve [10]. Still in the literature, there is an interesting study that opposes all the aforementioned data about the incidence of vagus cervical position. In their surgical dissections of 50 fresh cadavers, Hojaij et al. [11] used the carotid artery only as reference mark to identify a left sided anterior position of the vagus nerve in the astonishing 68% of the cases and also anterior position of the right vagus nerve in 12%! This paper is very well statistically tailored, however the pictures of limited neck dissection through a routine surgical incision do not demonstrate clearly this anterior position of the vagus nerve. It is also possible without complete neck dissection, ansa cervicalis superior root [4] or some of its branches descending along the common carotid artery to be erroneously counted for anterior vagus nerve.
Normal course of the vagus nerve and different unusual positions can be explained by studying its embryonic development. During 12-15 week of gestation, the vagus nerve shifted its position to the artery and vein from anterior, via intermediate, to posterior position, which is its definite position in adults [12]. This shifting corresponds to increasing in thickness of common carotid artery which can be a possible reason for this position changes. Another possible reason can be migrating upwards of sympathetic ganglia together with inferior vagal ganglion, producing dorsal traction [12]. However, on the left side this process lags, and in some cases the nerve stays anteriorly [12]. All the aforementioned facts can explain the anterior course of the vagus nerve as an imperfect posterior shifting, more often on the left side.
Conclusion
Surgeons performing cervical neck dissection have to be well aware of the normal course of the vagus nerve as well as its variations. This variation must be considered during carotid endarterectomy, where retraction, stretching, or clamping of the nerve can happen. Vagus nerve might be damaged during such neck dissection, which can present mainly with hoarseness, dysphagia and upper airway obstruction. In vagus neuromonitoring, surgeons must be aware for this anomaly as well.
REFERENCES
- Standring S (Ed.). Gray’s Anatomy - the Anatomical Basis of Clinical Practice. 41st Ed., London, Elsevier. 2016;466.
- Paulsen F, Waschke J. Sobotta Atlas of Human Anatomy. Head, Neck and Neuroanatomy. 15th Ed. Munich, Elsevier GmbH. 2011;169.
- Park JK, Jeong SY, Lee JH, et al. Variations in the course of the cervical vagus nerve on thyroid ultrasonography. AJNR Am J Neuroradiol. 2011;32:1178-81.
- AbuRahma AF, Lim RY. Management of vagus nerve injury afer carotid endarterectomy. Surg. 1996;119:245-7.
- Ballotta E, Da Giau G, Renon L, et al. Cranial and cervical nerve injuries after carotid endarterectomy: a prospective study. Surg. 1999;125:85-91.
- AbuRahma AF, Choueiri MA. Cranial and cervical nerve injuries after repeat carotid endarterectomy. J Vasc Surg. 2000;32:649-54.
- Giovagnorio F, Martinoli C. Sonography of the cervical vagus nerve: normal appearance and abnormal findings. AJR Am J Roentgenol. 2001;176:745-9.
- Dionigi G, Chiang FY, Rausei S, et al. Surgical anatomy and neurophysiology of the vagus nerve (VN) for standardised intraoperative neuromonitoring (IONM) of the inferior laryngeal nerve (ILN) during thyroidectomy. Langenbecks Arch Surg. 2010;395:893-9.
- Veleanu C, Dinulescu T, Zolog I. Vagus nerve passing in front of the left lobe of the thyroid gland. Anat Anz. 1977;141:84-5.
- Gibson A. Bilateral abnormal relationship of the vagus nerve in its cervical portion. J Anat Physiol. 1915;49:389-92.
- Hojaij F, Rebelo G, Akamatsu F, et al. Syntopy of vagus nerve in the carotid sheath: A dissectional study of 50 cadavers. LIO. 2019;4:319-22.
- Miyake N, Hayashi S, Kawase T, et al. Fetal anatomy of the human carotid sheath and structures in and around it. Anat Rec (Hoboken). 2010;293:438-45.