Using the Appendix as a Ureteral Substitute During Pyeloplasty in a Patient with Ureteropelvic Junction Obstruction
Received: 08-Apr-2022, Manuscript No. 4737; Editor assigned: 12-Apr-2022, Pre QC No. 4737; Accepted Date: Apr 28, 2022; Reviewed: 22-Apr-2022 QC No. 4737; Revised: 27-Apr-2022, Manuscript No. 4737; Published: 28-Apr-2022
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
A 21-year-old male presented for surgical management of a right-sided ureteropelvic junction obstruction. A dismembered pyeloplasty via a robotic-assisted laparoscopic approach was attempted, but the ureter could not be mobilized to perform a tension-free anastomosis. Ureteral reconstruction was necessary and use of small bowel was planned to replace the non-functional ureter. However, patient was noted to have a healthy and patent appendix, which was utilized in lieu of small bowel. The surgery was converted to an open procedure, and an appendiceal interposition was successfully performed. The patient’s immediate postoperative period was significant for a small urine leak, exacerbated by an episode of urinary retention, which was managed successfully with an indwelling urethral catheter and a ureteral stent. The rest of the patient’s postoperative course was uneventful, and he remains symptom-free at three-month follow-up. This case highlights the successful use of an appendiceal interposition for ureteral reconstruction in a patient who required a right-sided pyeloplasty for ureteropelvic junction obstruction.
Keywords
Ureteropelvic Junction Obstruction; Pyeloplasty; Appendix; Ureter; Appendiceal Interposition; Ureteral Reconstruction
Introduction
Ureteropelvic Junction Obstruction (UPJO) can be managed by a variety of strategies including surveillance, endoscopic approaches, and definitive repair. Choice of management typically depends on age at diagnosis and associated symptoms of urinary obstruction. When surgery is indicated, the preferred treatment approach is minimally invasive pyeloplasty. While the dismembered pyeloplasty is the preferred repair by most urologists, it may not be suitable in all clinical scenarios. We describe a case report of a robotic-assisted laparoscopic pyeloplasty converted to an open appendiceal interposition to supplement ureteral length.
Case
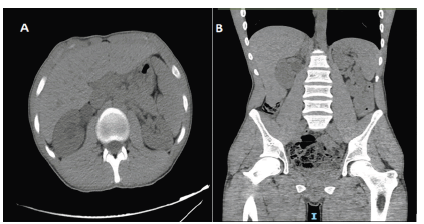
A 21-year-old male with no significant past medical history presented to the emergency room in December 2021 with worsening right flank pain over the course of two days. Physical exam was significant for right costovertebral angle tenderness. Laboratory values demonstrated a White Blood Count (WBC) of 18 × 103/microliter (µL) and urinalysis showed moderate leukocyte esterase and >50 WBC per high powered focus. Serum creatinine level was 1.01 milligrams per deciliter (mg/dL). A non-contrast Computed Tomography (CT) scan of the abdomen and pelvis (Figure 1) demonstrated right-sided hydronephrosis to the level of the Ureteropelvic Junction (UPJ).
Figure 1: Initial presentation on non-contrast Computed Tomography (CT) showing right-sided hydronephrosis down to the ureteropelvic junction on (A) axial (B) coronal scans.
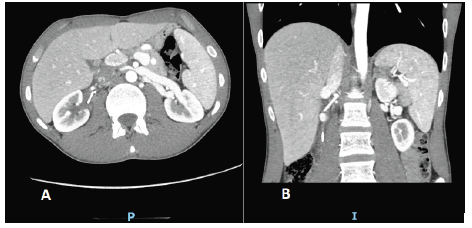
Given concern for urinary obstruction in the setting of an upper urinary tract infection, the patient was taken for urgent urinary decompression with cystoscopy and ureteral stent placement. A retrograde pyelogram performed during the procedure confirmed the presence of a right UPJO. After completion of a one-week antibiotic course, the patient was seen by one of our renal surgeons and underwent further workup. A CT angiogram (Figure 2) was performed which demonstrated mild right hydronephrosis down to the right UPJ with a branch of the main right renal artery traversing anterior to the renal pelvis, likely representing UPJO from a crossing vessel. The patient was recommended for treatment of the UPJO with robotic-assisted laparoscopic pyeloplasty.
Figure 2: Preoperative CT angiography demonstrating presence of a right renal accessory artery as well as an indwelling ureteral stent on (A) axial (B) coronal scans.
Surgery initially proceeded with the standard laparoscopic approach for renal surgery. The patient was positioned in the left lateral decubitus position and the operating room table flexed to extend the right flank. Three 8-millimeter (mm) robotic ports were placed along with a 12 mm assistant port and a 5 mm trocar for retracting the liver. The DaVinci robot was docked, and the surgery proceeded as expected with mobilization of the ascending colon and exposure of the plane between Gerota’s fascia and the mesocolon. The right ureter was identified and found to be encased in an inflammatory rind extending from below the iliac bifurcation up to the renal pelvis. A mildly hydronephrotic renal pelvis was seen and isolated. A small accessory arterial vessel was identified crossing over the UPJ. Under direct vision, the right UPJ was transected sharply and the renal pelvis was reduced. A 1-centimeter (cm) specimen of the UPJ was resected and sent for pathology. The renal pelvis was transposed in front of the crossing vessel. When reattachment of the remaining proximal right ureter with the renal pelvis was attempted, there was extensive inflammatory rind in the retroperitoneum, and the right ureter could not be safely mobilized to ensure a tension-free anastomosis. Because a dismembered pyeloplasty could not be performed, a small bowel interposition was initially planned. However, the patient was also noted to have a healthy appearing appendix of sufficient length for ureteral interposition. The DaVinci robot was undocked and a flank incision was made from the tip of the 12th rib towards the umbilicus. The appendix was again inspected and seen as a viable choice given its robust length and width. Using a GIA 60 mm stapler, the appendix was isolated from the cecum while preserving its blood supply. Both proximal and distal ends of the appendix was opened and all fecal material was washed out. The proximal segment of the appendix was spatulated and anastomosed to the right renal pelvis with interrupted Vicryl sutures. The distal end of the appendix as well as the proximal end of the right ureter were spatulated and anastomosed in a cobra head fashion using Vicryl sutures. A 6 French (Fr) × 26 cm ureteral stent was positioned within the reconstructed right ureter. The patient tolerated the procedure without issue and was discharged on postoperative day (POD) 2 after passing a trial of void.
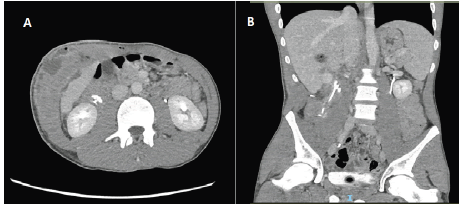
The patient presented to the hospital on POD 7 with gross hematuria and urinary retention. Patient’s labs demonstrated a serum creatinine level of 0.81 mg/dL, a hemoglobin level of 11.7 grams (g) /dL, and a WBC level of 18 × 103/µL. A CT Urogram (Figure 3) was performed showing contrast extravasation along the path of the right ureteral stent, suggestive of a urine leak. The patient was initiated on broad spectrum antibiotics and an indwelling urethral catheter was placed for urinary decompression. The ureteral stent was left in place. The patient clinically improved over the course of three days in the hospital, and the patient was discharged with antibiotics as well as the urethral catheter.
Figure 3: Delayed phase of a triphasic CT (Urogram) performed one week after surgery showed contrast extravasation around the indwelling ureteral stent on (A) axial (B) coronal scans.
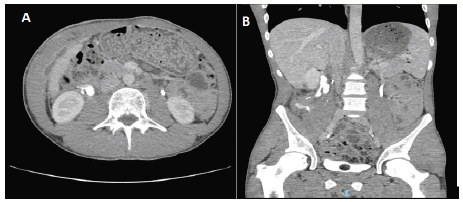
The patient had subsequent imaging with triphasic CT (Figure 4) performed on POD 14 which showed persistent contrast extravasation along the right ureteral stent. After completion of antibiotic course, the WBC level had decreased to 7 × 103/µL. The decision was made to remove the indwelling urethral catheter but leave the ureteral stent for a longer period of time. Eight weeks after surgery, the patient presented for cystoscopy to assess the integrity of his appendiceal ureter.
Figure 4: Delayed phase of a triphasic CT performed two weeks after surgery showed persistent contrast extravasation around indwelling ureteral stent on (A) axial (B) coronal scans.
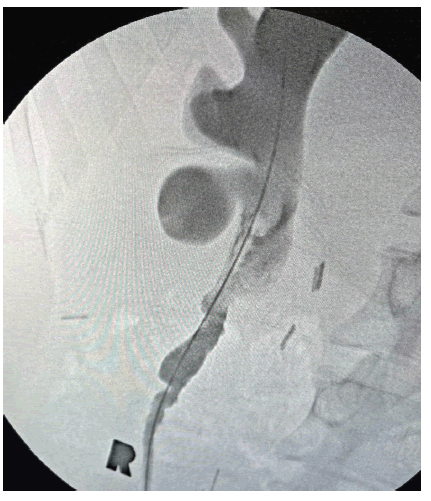
A retrograde pyelogram (Figure 5) was performed which showed no contrast extravasation from the appendiceal ureter, and the indwelling ureteral stent was removed. The patient remains symptoms-free at three months after surgery.
Figure 5: Right-sided retrograde pyelogram performed eight weeks after surgery showing no extravasation of contrast outside of the reconstructed ureter.
Discussion
We describe the case of a 21-year-old man who was found to have a symptomatic right UPJO and underwent treatment with pyeloplasty and appendiceal interposition. A UPJO is a partial or complete blockage of urinary flow from the renal pelvis into the ureter. The etiology of this obstruction can be congenital or acquired. Congenital causes of obstruction can include intrinsic stenosis of the proximal ureter where the normal musculature of the ureter is replaced by abnormal muscle bundles or fibrous tissue, eliminating the normal peristalsis of the ureter [1]. Acquired causes can include kidney stones, iatrogenic sources, or malignancy.
Congenital UPJO can also develop from compression of the UPJ from an external structure, usually an accessory vessel from the renal artery. However, there is controversy whether compression from the crossing vessel itself is the cause of the obstruction. The true cause of obstruction may be intrinsic disease at the UPJ [2]. However, a review of histopathology from 95 patients with UPJO found that 43% patients with a crossing vessel had no intrinsic abnormality [3]. Additionally, studies have found that the presence of crossing vessels decreases the effectiveness of endoscopic procedures in the treatment of UPJO [4, 5].
While most cases are congenital, a UPJO may not become apparent until later in life when symptoms arise [6]. UPJ obstruction is the most common cause of prenatal hydronephrosis and can be found in up to 30% of patients with urinary tract dilation on prenatal ultrasound [7]. If prenatal screening is not performed, younger children can present with symptoms of urinary tract infection, palpable abdominal mass, hematuria, or failure to thrive. Older children or adults, on the other hand, are more likely to present with symptoms of intermittent flank pain, abdominal pain, or Dietl’s crisis [8]. Radiographic studies should be performed to determine the anatomic location as well as the functional significance of the obstructed UPJ.
Intervention is typically indicated when the patient develops symptoms associated with obstruction, impairment of renal function, or development of urinary tract infections or nephrolithiasis. Minimally symptomatic UPJ can be observed since majority of patients (>70%) may not require surgery over a period of 4 years [9]. Endoscopic techniques, such as endopyelotomy, can also treat UPJO. However, the success rate of endopyelotomy is limited by the presence of other factors like a high degree of obstruction or a crossing vessel. When treatment is warranted, the dismembered pyeloplasty is the procedure of choice for most cases of UPJO [10, 11]. Historically, a pyeloplasty was performed via an open approach, but currently, minimally invasive surgery has become the preferred approach in both adult and pediatric populations [12, 13]. Open and minimally invasive pyeloplasty have comparable outcomes, but both have significantly higher success rates than endopyelotomy [14].
While a minimally-invasive pyeloplasty was attempted in our patient, it became apparent during the surgery that additional ureteral length was needed, so an appendiceal interposition was performed as a ureteral substitute. An appendiceal ureter is typically used for proximal or mid-ureteral strictures [15]. It is a good alternative over a small bowel interposition since it does not require additional bowel anastomoses and decreases the risk for postoperative bowel complications. However, the appendix cannot be definitively used in every scenario since it needs to be assessed during surgery to ensure the length and caliber are appropriate [16]. Options for an appendiceal ureter include performing an interposition or an onlay technique. The interposition technique uses an appendix that is left tubularized and bridges a prior segment of ureter that was resected. The onlay technique involves spatulating the antimesenteric border of the appendix and then augmenting the ureteral lumen. There are limited studies to suggest which technique is better, but some surgeons prefer the onlay technique whenever possible to avoid anastomotic strictures due to the narrow lumen of the appendix [16, 17].
In our patient, an appendiceal onlay flap would not have been possible given the resection performed over the diseased portion of the UPJ, so a ureteral substitute was needed. Outcome data following ureteral reconstruction with an appendiceal ureter is limited; the majority of the literature consists of case reports or studies with relatively small sample sizes. These reports cite success rates of appendiceal interposition ranging from 92%-100% [17-22]. Our patient demonstrated a urine leak in the immediate postoperative period after experiencing hematuria and acute urinary retention. The urine leak was most likely secondary to retrograde reflux of urine up the ureteral stent in the setting of urinary retention causing weakening of the ureteral-appendiceal anastomosis. There are no reports in the literature of patients who developed urine leaks after an appendiceal interposition for ureteral reconstruction. Nevertheless, management of an upper tract urine leak typically involves placement of a urethral catheter with or without a ureteral stent which lowers the upper tract urinary pressures that could theoretically worsen the leak [23]. Our patient had successful resolution of a small postoperative urine leak using conservative measures; placement of a urethral catheter for one week and leaving the ureteral stent for eight weeks resolved the urine leak. Overall, the appendiceal ureter was successfully performed and helped bridge the gap in ureteral length that was needed for this patient during a pyeloplasty procedure.
Conclusion
We present the unique case of a patient who underwent surgical repair of a right-sided UPJO. However, the patient’s retroperitoneal anatomy precluded a simple pyeloplasty. Ureteral reconstruction was necessary and performed with an appendiceal interposition. While the immediate postoperative period was significant for a urine leak, which was exacerbated by acute urinary retention, the patient was successfully managed conservatively with a urethral catheter and a ureteral stent. Postoperative outcomes at three months follow-up demonstrate that the appendix is a viable option to restore ureteral continuity.
REFERENCES
- Hanna MK, Jeffs RD, Sturgess JM, et al. Ureteral structure and ultrastructure. Part II. Congenital ureteropelvic junction obstruction and primary obstructive megaureter. J Urol. 1976; 116 (6):725-30.
Google Scholar Crossref - Hanna MK. Some observations on congenital ureteropelvic junction obstruction. Urology. 1978; 12 (2):151-9.
Google Scholar Crossref - Richstone L, Seideman CA, Reggio E, et al. Pathologic findings in patients with ureteropelvic junction obstruction and crossing vessels. Urology. 2009; 73 (4):716-9.
Google Scholar Crossref - Van Cangh PJ, Wilmart JF, Opsomer RJ, et al. Long-term results and late recurrence after endoureteropyelotomy: a critical analysis of prognostic factors. J Urol. 1994; 151 (4):934-7.
Google Scholar Crossref - Nakada SY, Wolf JS, Brink JA, et al. Retrospective analysis of the effect of crossing vessels on successful retrograde endopyelotomy outcomes using spiral computerized tomography angiography. J Urol. 1998; 159 (1):62-5.
Google Scholar Crossref - Jacobs JA, Berger BW, Goldman SM, et al. Ureteropelvic obstruction in adults with previously normal pyelograms: a report of 5 cases. J Urol. 1979; 121 (2):242-44.
Google Scholar Crossref - Nguyen HT, Benson CB, Bromley B, et al. Multidisciplinary consensus on the classification of prenatal and postnatal urinary tract dilation (UTD classification system). J Pediatr Urol. 2014; 10 (6):982-98.
Google Scholar Crossref - Gonzalez R, Schimke CM. Ureteropelvic junction obstruction in infants and children. Pediatr Clin North Am. 2001; 48 (6):1505-18.
Google Scholar Crossref - Gurbuz C, Best SL, Donnally C, et al. Intermediate term outcomes associated with the surveillance of ureteropelvic junction obstruction in adults. J Urol. 2011; 185 (3):926-9.
Google Scholar Crossref - O'Reilly PH. Functional outcome of pyeloplasty for ureteropelvic junction obstruction: prospective study in 30 consecutive cases. J Urol. 1989; 142 (2 Pt 1):273-6.
Google Scholar Crossref - Clark WR, Malek RS. Ureteropelvic junction obstruction. I. Observations on the classic type in adults. J Urol. 1987; 138 (2):276-9.
Google Scholar Crossref - Jacobs BL, Kaufman SR, Morgenstern H, et al. Trends in the treatment of adults with ureteropelvic junction obstruction. J Endourol. 2013; 27 (3):355-60.
Google Scholar Crossref - Jacobs BL, Lai JC, Seelam R, et al. Variation in the Use of Open Pyeloplasty, Minimally Invasive Pyeloplasty, and Endopyelotomy for the Treatment of Ureteropelvic Junction Obstruction in Adults. J Endourol. 2017; 31 (2):210-5.
Google Scholar Crossref - Jacobs BL, Lai JC, Seelam R, et al. The Comparative Effectiveness of Treatments for Ureteropelvic Junction Obstruction. Urology. 2018;111:72-7.
Google Scholar Crossref - Bilotta A, Wiegand LR, Heinsimer KR. Ureteral reconstruction for complex strictures: a review of the current literature. Int Urol Nephrol. 2021;53(11):2211-9.
Google Scholar Crossref - Duty BD, Kreshover JE, Richstone L, et al. Review of appendiceal onlay flap in the management of complex ureteric strictures in six patients. BJU Int. 2015;115(2):282-7.
Google Scholar Crossref - Jun MS, Stair S, Xu A, et al. A Multi-Institutional Experience With Robotic Appendiceal Ureteroplasty. Urology. 2020;145:287-91.
Google Scholar Crossref - Dagash H, Sen S, Chacko J, et al. The appendix as ureteral substitute: a report of 10 cases. J Pediatr Urol. 2008;4(1):14-9.
Google Scholar Crossref - Cao H, Zhou H, Yang F, et al. Laparoscopic appendiceal interposition pyeloplasty for long ureteric strictures in children. J Pediatr Urol. 2018;14(6):551 e1- e5.
Google Scholar Crossref - Yarlagadda VK, Nix JW, Benson DG, et al. Feasibility of Intracorporeal Robotic-Assisted Laparoscopic Appendiceal Interposition for Ureteral Stricture Disease: A Case Report. Urology. 2017; 109: 201-5.
Google Scholar Crossref - Antonelli A, Zani D, Dotti P, et al. Use of the appendix as ureteral substitute in a patient with a single kidney affected by relapsing upper urinary tract carcinoma. Sci. World J. 2005; 5: 276-9.
Google Scholar Crossref - Thomas A, Eng MM, Hagan C, et al. Appendiceal substitution of the ureter in retroperitoneal fibrosis. J Urol. 2004; 171(6 Pt 1):2378.
Google Scholar Crossref - Ghavamian R, Chalouhy C. Complications of Urologic Surgery. 2021. In: Campbell-Walsh-Wein Urology. Philadelphia, PA: Elsevier. 12: 260-81.
Google Scholar Crossref