Variability in blood pressure and heart rate during dental surgery
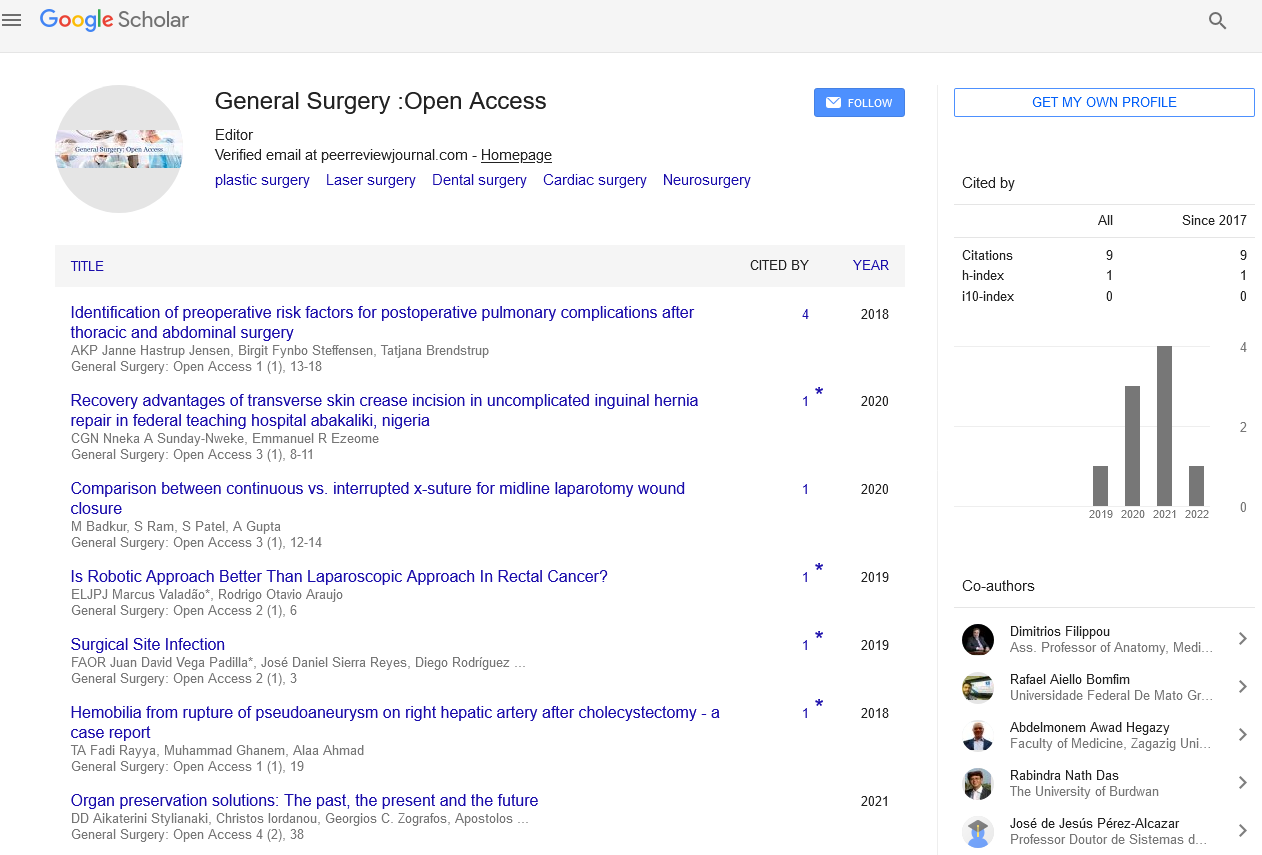
Received: 22-Mar-2022, Manuscript No. PULGSOA-22-4532; Editor assigned: 24-Mar-2022, Pre QC No. PULGSOA-22-4532(PQ); Accepted Date: Mar 26, 2022; Reviewed: 26-Mar-2022 QC No. PULGSOA-22-4532(Q); Revised: 26-Mar-2022, Manuscript No. PULGSOA-22-4532; Published: 28-Mar-2022, DOI: 10.37532/pulgsoa.2022.5(2):4-5.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Opinion
Many dental clinic patients have systemic disorders such as hypertension, ischemic heart disease, and other atherosclerotic conditions. In one research, 64% of older patients who attended the dental clinic were found to have one or more systemic disorders; hypertension was the most frequent, affecting up to 30% of the patients. Most dental procedures are performed under local anesthetic, and blood pressure elevations have been documented during tooth extraction even in normotensive individuals. Previous research in our lab found that a rise in blood pressure during tooth extraction is related to the difficulty of the extraction and the volume of local anesthetic utilized. Furthermore, blood pressure changes during an extraction process are age-dependent; middle-aged and older people have a larger increase in blood pressure during dental surgery than younger ones. However, the reaction of blood pressure during tooth extraction in hypertensive individuals has not been studied. It is critical to investigate the effects of dental surgery on blood pressure response in hypertensive individuals since a deadly cerebral hemorrhage and extensive bleeding have been linked to dental surgery and hypertension. Power spectral analysis of R-R variability has been frequently utilized to assess the contributions of the sympathetic and parasympathetic nervous systems to cardiac activity. Although increased sympathetic neural activity has been documented in essential hypertension, serial changes in sympathetic and parasympathetic nerve activity after dental surgery have yet to be confirmed. We expected that tooth extraction increases sympathetic nervous system activity in hypertension individuals, resulting in an increased pressor reaction. It is well established that patient age has a significant effect on heart rate variability and blood pressure responses. As a result, in this study, we compared changes in blood pressure and heart rate variability in hypertension patients to those in age and gender-matched normotensive individuals after dental surgery.
Most dental procedures cause a significant cardiovascular reaction, which is normally innocuous in healthy people but might be quite harmful in vulnerable patients with heart problems. Acute psychological stress, such as that encountered during a dental procedure, induces a defensive response defined by an increase in sympathetic nerve activity, which may precipitate unfavorable cardiac events in individuals with severe heart failure. Clinicians require a criterion for the early detection of an increased increase in heart activity owing to an enhanced sympathetic drive to terminate a dental operation before a life-threatening cardiovascular event occurs. Blood Pressure (BP) and Heart Rate (HR) are commonly used as indirect indicators of increased sympathetic activity during stress; however, research has not proven the actual validity of these parameters in the early detection of abnormal cardio-circulatory changes that may occur in cardiac emergencies. Indeed, HR and blood pressure patterns under stressful circumstances are determined by the normal behavior of the individual in the situation. A common rise in peripheral vascular resistance in some persons causes a prolonged increase in BP, which is responsible for a decrease in HR via baroreflex-mediated processes, whereas a common increase in cardiac response in others causes an increase in HR as well as a decrease in BP. As a result, HR and BP alone or in combination should not be regarded as valid indicators for evaluating cardiovascular activity during stress, because they frequently interact with each other and are inversely associated. Heart rate variability, or HRV, has been recognized as one of the most promising measures of cardiovascular function by researchers. HRV is measured by analyzing successive sinus rhythm R-R intervals (beat to beat) and may offer quantitative information on the modulation of cardiac vagal and sympathetic nerve activity to the heart.
Low HRV levels suggest higher sympathetic cardiac activity and an increased risk of malignant dysrhythmias, especially in heart disease patients. Researchers have shown that a stressful scenario, such as a dentist appointment, has a large impact on HRV and have proposed that it might be a sensitive quantitative measure of autonomic activity under stress. The goal of this study was to compare the sensitivity of HRV in assessing the cardiocirculatory response during a tooth extraction to other clinical indicators that are more commonly utilized in clinical practice.
Each patient was asked to fill out a questionnaire on their medical history and medication use on the day of their dental surgery. Following the recording of a 12-lead ECG, continuous two-channel Holter electrocardiographic monitoring was commenced, with the findings taped. Patients were placed in a supine posture in a silent room for at least 10 minutes, and blood pressure and pulse rate were taken every 2 minutes using an oscillometric technique and automated equipment. The baseline blood pressure and pulse rate were established as the averages of the previous two readings. Patients were then sent to the dental department for tooth extraction. Patients were kept in a supine position for the duration of the therapy. After at least 10 minutes of control, a local anesthetic was delivered. All patients were given lignocaine 2% with adrenaline (1: 80000) as an anesthetic. The surgery began 10 minutes after the local anesthetic was administered. Patients were maintained in a supine position for at least 10 minutes following surgery. Throughout the trial, blood pressure and pulse rate were recorded every 2 minutes. For additional investigation, blood pressure and pulse rate were averaged in each patient during each treatment phase (before surgery, during local anesthetic, during surgery, and after surgery). To exclude the impacts of surgery length or local anesthetic volume, we used data from the first 10 minutes after dental surgery in the current investigation.
The current study's two main findings are those blood pressure responses during dental surgery did not differ between normotensive and hypertension individuals, and that the reactions of the cardiac sympathetic and parasympathetic nervous systems differed between the two groups. This is, to the best of our knowledge, the first study to look into the power spectrum analysis of R-R variability during dental surgery in hypertension individuals. Few researches have been done to examine how blood pressure varies in hypertensive individuals during dental surgery. Abraham-Inpijn et al. discovered that blood pressure raises more in hypertension individuals than in normotensive patients during dental treatments.
However, they did not control for patient age in their study; given that older patients had higher baseline blood pressure and bigger variations in blood pressure during dental surgery, their results might have been impacted by the patients' age. Meyer, on the other hand, revealed that blood pressure and heart rate alterations caused by tooth extraction are identical in normotensive and hypertension individuals. In the current study, patient variables such as age and gender were corrected for normotensive and hypertensive patients, and all patients had their teeth extracted by the same dentist. After controlling for patient characteristics and surgical bias, there was no difference in blood pressure response during dental surgery between normotensive and hypertension patients.
The cardiovascular response to a stressful event is assumed to be impacted by cardiac-vagal withdrawal and adrenergic activation, which results in enhanced cardiac chronotropic and inotropic effects (cardiac reaction) as well as increased total peripheral resistance (vascular reaction). As a result, both HR and blood pressure rise. However, the hemodynamic underpinning cardiovascular responses to mental stress activities would necessarily differ between persons and tasks. People differ in the cardiac and vascular mechanisms that underpin their cardiovascular response to a stressful circumstance, and their reactions may be distinguished by the amount to which they include a primary increase in cardiac output (cardiac reactors) or peripheral resistance (vascular reactors). It is now known that some persons are principally cardiac responders; while others are vascular reactors and that some tasks evoke cardiac reactions while others elicit vascular reactions.
These findings indicate that, while a subject's hemodynamic responses to behavioral stimuli vary, the diversity between persons is constant. Individual variations in sympathoadrenal activation (epinephrine vs norepinephrine) under a stressful scenario may indicate disparities in cardiac and vascular response.