Variations in the cubital fossa
Sharmistha Biswas1*,Anjan Adhikari2 and PanchananKundu1
1Department of Anatomy, Bankura Sammilani Medical College, Bankura, West Bengal,India
2Department of Pharmacology, R.G.Kar Medical College, Kolkata,India
- *Corresponding Author:
- Dr. Sharmistha Biswas, MS
Assistant Professor, Department of Anatomy, Bankura Sammilani Medical College, Bankura, West Bengal, India.
Tel: +91 990 3408977
E-mail: drsharmisthabiswas@rediffmail.com
Date of Received: April 23rd, 2010
Date of Accepted: August 6th, 2010
Published Online: August 19th, 2010
© IJAV. 2010; 3: 122–124.
[ft_below_content] =>Keywords
median nerve,cubital fossa,accessory slip of brachialis muscle,brachial artery
Introduction
The brachial artery begins as a continuation of the axillary artery and is superficial throughout its course in the arm. When it enters the cubital fossa it lies anterior to the brachialis muscle and lateral to the median nerve. In cubital fossa it lies deep to bicipital aponeurosis which separates the artery from median cubital vein. The median nerve descends along the lateral side of the proximal part of brachial artery. At the middle of the arm the nerve crosses from lateral to medial, usually in front of the artery and then passes along the medial side of the brachial artery. It appears in cubital fossa beneath the bicipital aponeurosis and rests on the brachialis. In cubital fossa, usually the structures lying from lateral to medial are tendon of biceps brachii, brachial artery and median nerve (TAN). No literature is available stating median nerve to be lateral to the brachial artery in cubital fossa.
Both brachial artery and median nerve lie superficial to the brachialis muscle in the front of arm. But authors like Bilecenoglu et al. and George & Nayak described abnormal slip arising from brachialis muscle passing superficial to and causing entrapment of the nerve and the artery [1,2]. Loukas et al. reported a case of an accessory brachialis muscle, which originated medially from the mid-shaft of the humerus and the medial intermuscular septum [3]. During its course medially, toward the elbow, it crossed both the brachial artery and the median nerve.
Case Report
During routine dissection of a 60-year-old East Indian female cadaver for undergraduate teaching in the Department of Anatomy, Bankura Sammilani Medical College, West Bengal, India, we came across some interesting variations.
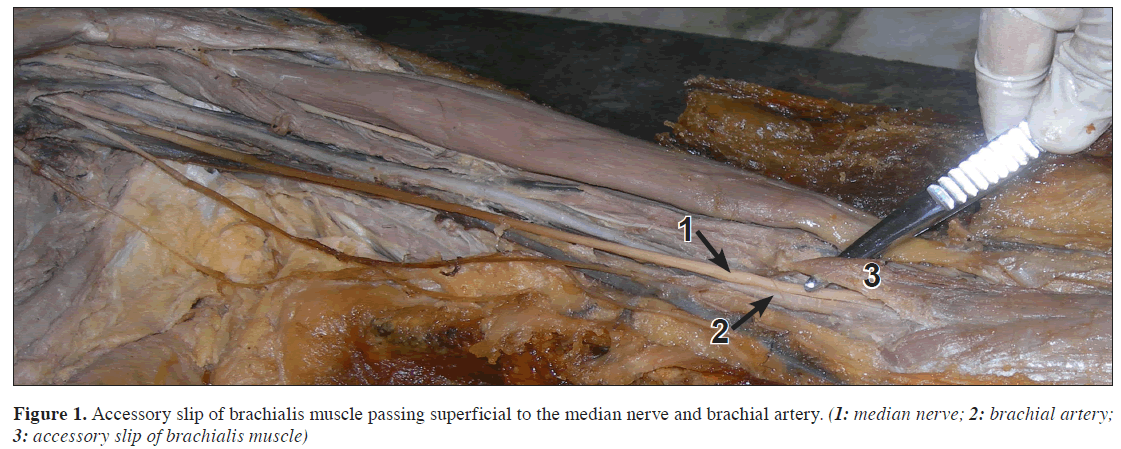
In the front of the arm, from the distal part of brachialis muscle a few fleshy fibers diverged and were found to blend with common origin of flexor muscles after an oblique course. The median nerve and brachial artery were found to be normal in the upper part of their course in the arm. In the lower part, instead of passing superficial to brachialis, both of them passed deep to the accessory slip of brachialis muscle (Figure 1).
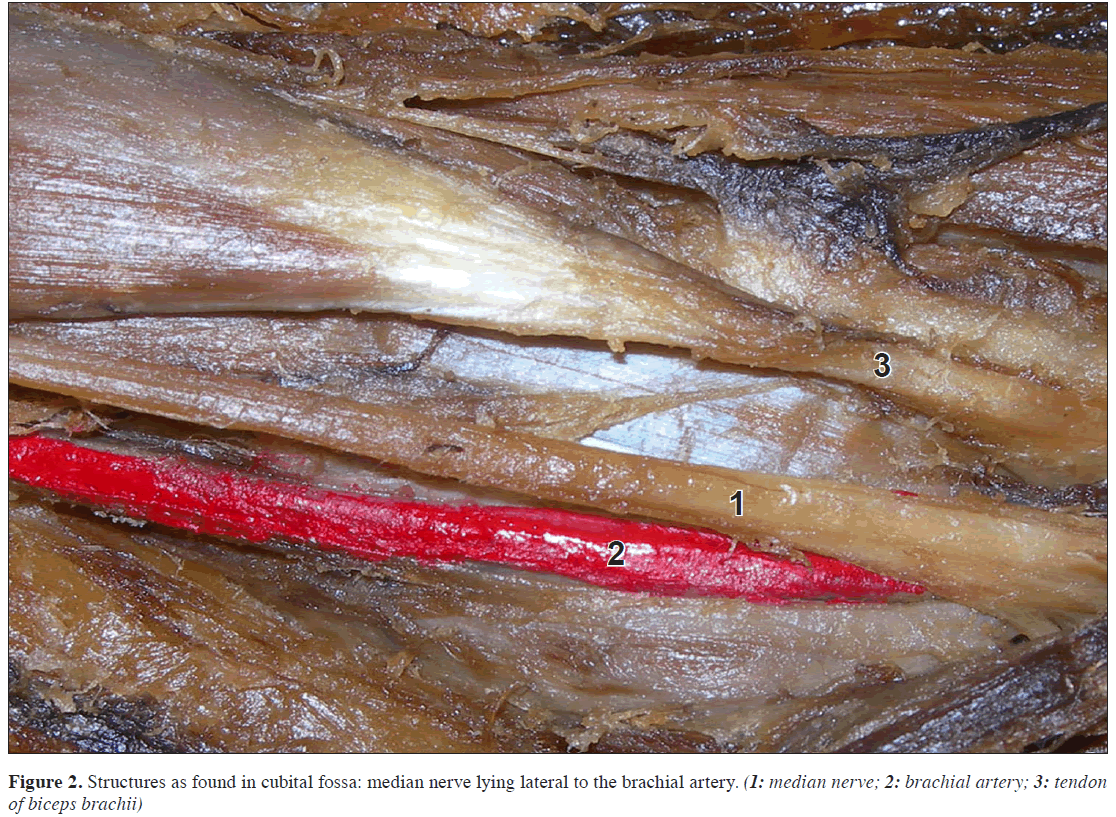
After cutting the slip to reveal the subsequent course of the neurovascular bundle, it was found that the median nerve passed medial to the brachial artery (Figure 2). In the cubital fossa, the structures lying from lateral to medial were tendon of biceps brachii, median nerve and brachial artery, instead of the usual TAN (tendon, artery, nerve) arrangement.
In cubital fossa, 1.25 cm below line of elbow joint, the artery divided into radial and ulnar artery as usual, which then followed their usual course and branching pattern. The median nerve also followed normal course and branching pattern in the forearm.
The variations were found in both the upper limbs.
Discussion
We observed that from lower part of the brachialis muscle, an accessory fleshy slip passed obliquely downwards and medially to merge with the common origin of the superficial flexors. The brachial artery and the median nerve passed below this slip.
Our findings were similar to that of Loukas et al., who reported a case of an accessory brachialis muscle that originated medially from the mid-shaft of the humerus and the medial intermuscular septum [3]. During its course medially, toward the elbow, it crossed both the brachial artery and the median nerve. The distal tendon split to surround the median nerve before inserting into the common tendon of the antebrachial flexor compartment muscles.
According to Bilecenoglu et al., there are 7 possible compression sites for the median nerve : brachialis (1), Struthers’ ligament (2), bicipital aponeurosis (3), pronator teres (4), flexor digitorum superficialis (5), vascular structures (6), accessory head of flexor pollicis longus (Gantzer’s muscle) (7) [1]. They commented that the median nerve may be compressed above the elbow because of an accessory tendon which arises from the brachialis in 10% of the cases.
George and Nayak reported a case of median nerve and brachial artery entrapment in an additional slip of brachialis muscle, which could cause compression neuropathy of median nerve and vascular compression symptoms due to entrapment of the artery [2].
Rodrigues et al. found a variation in the insertion pattern of coracobrachialis and entrapped median nerve and brachial artery by the tendinous arch of the muscle, in relation to the neurovascular bundle [4].
The median nerve and the brachial artery were also similarly prone to get compressed by the accessory slip of brachialis muscle in the present case.
The percutaneous brachial approach is commonly used for carotid and vertebral angiography. Despite the adjacency of the brachial artery and median nerve in the cubital fossa, the complication rate of median nerve injury has been low. The maximal prevalence was 0.6% in brachial catheterization by arterial cut-down and brachial arteriotomy [5].
In our case of median nerve lying lateral to the brachial artery in the cubital fossa, possibility of median nerve injury during the procedure would be very high. Therefore, the responsible physician must be alert of the potential median nerve injury in this procedure, and sonographically guided brachial arterial puncture should be considered [6].
Embryological explanations
In man, the forelimb muscles develop from the mesenchyme of the para-axial mesoderm during fifth week of embryonic life [7]. The precursors of the musculoskeletal lineage are derived from the myotome of the somite. Myoblasts are stimulated to migrate into the developing limb buds by several growth factors produced by cells in the proximal limb bud. These premuscle cells express adhesion molecules that are important in properly distributing them throughout the limb [8]. The presence of an accessory slip of brachialis muscle may indicate alterations in the formation and structure of the myotome or somite, or in the distribution of the cell adhesion molecules present on the premuscle cells.
The interpretation of the nerve anomaly of the arm requires consideration of the phylogeny and development of the nerves of the upper limb. The axons of spinal nerves grow distally to reach the limb bud mesenchyme. As the guidance of the developing axons is regulated by expression of chemoattractants and chemorepulsants in a highly coordinated, site-specific fashion any alterations in signal between mesenchymal cells and neuronal growth cones can lead to significant variations [9].
It can be concluded that the present case of bilateral variations in the course of median nerve and brachial artery (nerve lateral to artery) in the cubital fossa, both of which also passed deep to the accessory slip of brachialis muscle in the lower arm, is a very rare anomaly. Compression neuropathy of median nerve and vascular compression, as well as injury to the median nerve during brachial catheterization can occur in such a case. Another possible clinical consequence that could arise is irregularities in blood pressure measurements due to compression of the brachial artery by the additional slip of brachialis muscle.
References
- Bilecenoglu B, Uz A, Karalezli N. Possible anatomic structures causing entrapment neuropathies of the median nerve: An anatomic study. Acta Orthop Belg. 2005; 71: 169–176.
- George BM, Nayak SB. Median nerve and brachial artery entrapment in the abnormal brachialis muscle – a case report. Neuroanatomy. 2008; 7: 41–42.
- Loukas M, Louis RG Jr, South G, Alsheik E, Christopherson C. A case of an accessory brachialis muscle. Clin Anat. 2006; 19: 550–553.
- Rodrigues V, Nayak S, Nagabhooshana S, Vollala VR. Median nerve and brachial artery entrapment in the tendinous arch of coracobrachialis muscle. International Journal of Anatomical Variations. 2008; 1: 28–29.
- Macon WL IV, Futrell JW. Median-nerve neuropathy after percutaneous puncture of the brachial artery in patients receiving anticoagulants. N Engl J Med. 1973; 288: 1396.
- Chuang YM, Luo CB, Chou YH, Cheng YC, Chang CY, Chiou HJ. Sonographic diagnosis and treatment of a median nerve epineural hematoma caused by brachial artery catheterization. J Ultrasound Med. 2002; 21: 705–708.
- Larsen WJ. Human Embryology. 2nd Ed., Edinburgh, Churchill Livingstone. 1997; 311–339.
- Carlson BM. Human embryology and developmental biology. Philadelphia, Mosby. 2004; 224–225.
- Sannes HD, Reh TA, Harris WA. Development of the nervous system. New York, Academic Press. 2000; 189–197.
Sharmistha Biswas1*,Anjan Adhikari2 and PanchananKundu1
1Department of Anatomy, Bankura Sammilani Medical College, Bankura, West Bengal,India
2Department of Pharmacology, R.G.Kar Medical College, Kolkata,India
- *Corresponding Author:
- Dr. Sharmistha Biswas, MS
Assistant Professor, Department of Anatomy, Bankura Sammilani Medical College, Bankura, West Bengal, India.
Tel: +91 990 3408977
E-mail: drsharmisthabiswas@rediffmail.com
Date of Received: April 23rd, 2010
Date of Accepted: August 6th, 2010
Published Online: August 19th, 2010
© IJAV. 2010; 3: 122–124.
Abstract
The median nerve crosses in front of the brachial artery at the middle of the arm from lateral to medial side, and passes along its medial side. They appear in cubital fossa beneath bicipital aponeurosis and rest on brachialis muscle. In cubital fossa, structures lying from lateral to medial are tendon of biceps brachii, brachial artery and median nerve (TAN). No literature is available stating median nerve to be lateral to the brachial artery in the cubital fossa. In the present case, we found bilateral variations in the course of median nerve and brachial artery in the cubital fossa. The nerve was lateral to the artery. Both the structures passed deep to an accessory slip of brachialis muscle in the lower arm. It is a rare variation. Compression neuropathy of median nerve, vascular compression and injury to the median nerve during brachial catheterization can occur in such a case.
-Keywords
median nerve,cubital fossa,accessory slip of brachialis muscle,brachial artery
Introduction
The brachial artery begins as a continuation of the axillary artery and is superficial throughout its course in the arm. When it enters the cubital fossa it lies anterior to the brachialis muscle and lateral to the median nerve. In cubital fossa it lies deep to bicipital aponeurosis which separates the artery from median cubital vein. The median nerve descends along the lateral side of the proximal part of brachial artery. At the middle of the arm the nerve crosses from lateral to medial, usually in front of the artery and then passes along the medial side of the brachial artery. It appears in cubital fossa beneath the bicipital aponeurosis and rests on the brachialis. In cubital fossa, usually the structures lying from lateral to medial are tendon of biceps brachii, brachial artery and median nerve (TAN). No literature is available stating median nerve to be lateral to the brachial artery in cubital fossa.
Both brachial artery and median nerve lie superficial to the brachialis muscle in the front of arm. But authors like Bilecenoglu et al. and George & Nayak described abnormal slip arising from brachialis muscle passing superficial to and causing entrapment of the nerve and the artery [1,2]. Loukas et al. reported a case of an accessory brachialis muscle, which originated medially from the mid-shaft of the humerus and the medial intermuscular septum [3]. During its course medially, toward the elbow, it crossed both the brachial artery and the median nerve.
Case Report
During routine dissection of a 60-year-old East Indian female cadaver for undergraduate teaching in the Department of Anatomy, Bankura Sammilani Medical College, West Bengal, India, we came across some interesting variations.
In the front of the arm, from the distal part of brachialis muscle a few fleshy fibers diverged and were found to blend with common origin of flexor muscles after an oblique course. The median nerve and brachial artery were found to be normal in the upper part of their course in the arm. In the lower part, instead of passing superficial to brachialis, both of them passed deep to the accessory slip of brachialis muscle (Figure 1).
After cutting the slip to reveal the subsequent course of the neurovascular bundle, it was found that the median nerve passed medial to the brachial artery (Figure 2). In the cubital fossa, the structures lying from lateral to medial were tendon of biceps brachii, median nerve and brachial artery, instead of the usual TAN (tendon, artery, nerve) arrangement.
In cubital fossa, 1.25 cm below line of elbow joint, the artery divided into radial and ulnar artery as usual, which then followed their usual course and branching pattern. The median nerve also followed normal course and branching pattern in the forearm.
The variations were found in both the upper limbs.
Discussion
We observed that from lower part of the brachialis muscle, an accessory fleshy slip passed obliquely downwards and medially to merge with the common origin of the superficial flexors. The brachial artery and the median nerve passed below this slip.
Our findings were similar to that of Loukas et al., who reported a case of an accessory brachialis muscle that originated medially from the mid-shaft of the humerus and the medial intermuscular septum [3]. During its course medially, toward the elbow, it crossed both the brachial artery and the median nerve. The distal tendon split to surround the median nerve before inserting into the common tendon of the antebrachial flexor compartment muscles.
According to Bilecenoglu et al., there are 7 possible compression sites for the median nerve : brachialis (1), Struthers’ ligament (2), bicipital aponeurosis (3), pronator teres (4), flexor digitorum superficialis (5), vascular structures (6), accessory head of flexor pollicis longus (Gantzer’s muscle) (7) [1]. They commented that the median nerve may be compressed above the elbow because of an accessory tendon which arises from the brachialis in 10% of the cases.
George and Nayak reported a case of median nerve and brachial artery entrapment in an additional slip of brachialis muscle, which could cause compression neuropathy of median nerve and vascular compression symptoms due to entrapment of the artery [2].
Rodrigues et al. found a variation in the insertion pattern of coracobrachialis and entrapped median nerve and brachial artery by the tendinous arch of the muscle, in relation to the neurovascular bundle [4].
The median nerve and the brachial artery were also similarly prone to get compressed by the accessory slip of brachialis muscle in the present case.
The percutaneous brachial approach is commonly used for carotid and vertebral angiography. Despite the adjacency of the brachial artery and median nerve in the cubital fossa, the complication rate of median nerve injury has been low. The maximal prevalence was 0.6% in brachial catheterization by arterial cut-down and brachial arteriotomy [5].
In our case of median nerve lying lateral to the brachial artery in the cubital fossa, possibility of median nerve injury during the procedure would be very high. Therefore, the responsible physician must be alert of the potential median nerve injury in this procedure, and sonographically guided brachial arterial puncture should be considered [6].
Embryological explanations
In man, the forelimb muscles develop from the mesenchyme of the para-axial mesoderm during fifth week of embryonic life [7]. The precursors of the musculoskeletal lineage are derived from the myotome of the somite. Myoblasts are stimulated to migrate into the developing limb buds by several growth factors produced by cells in the proximal limb bud. These premuscle cells express adhesion molecules that are important in properly distributing them throughout the limb [8]. The presence of an accessory slip of brachialis muscle may indicate alterations in the formation and structure of the myotome or somite, or in the distribution of the cell adhesion molecules present on the premuscle cells.
The interpretation of the nerve anomaly of the arm requires consideration of the phylogeny and development of the nerves of the upper limb. The axons of spinal nerves grow distally to reach the limb bud mesenchyme. As the guidance of the developing axons is regulated by expression of chemoattractants and chemorepulsants in a highly coordinated, site-specific fashion any alterations in signal between mesenchymal cells and neuronal growth cones can lead to significant variations [9].
It can be concluded that the present case of bilateral variations in the course of median nerve and brachial artery (nerve lateral to artery) in the cubital fossa, both of which also passed deep to the accessory slip of brachialis muscle in the lower arm, is a very rare anomaly. Compression neuropathy of median nerve and vascular compression, as well as injury to the median nerve during brachial catheterization can occur in such a case. Another possible clinical consequence that could arise is irregularities in blood pressure measurements due to compression of the brachial artery by the additional slip of brachialis muscle.
References
- Bilecenoglu B, Uz A, Karalezli N. Possible anatomic structures causing entrapment neuropathies of the median nerve: An anatomic study. Acta Orthop Belg. 2005; 71: 169–176.
- George BM, Nayak SB. Median nerve and brachial artery entrapment in the abnormal brachialis muscle – a case report. Neuroanatomy. 2008; 7: 41–42.
- Loukas M, Louis RG Jr, South G, Alsheik E, Christopherson C. A case of an accessory brachialis muscle. Clin Anat. 2006; 19: 550–553.
- Rodrigues V, Nayak S, Nagabhooshana S, Vollala VR. Median nerve and brachial artery entrapment in the tendinous arch of coracobrachialis muscle. International Journal of Anatomical Variations. 2008; 1: 28–29.
- Macon WL IV, Futrell JW. Median-nerve neuropathy after percutaneous puncture of the brachial artery in patients receiving anticoagulants. N Engl J Med. 1973; 288: 1396.
- Chuang YM, Luo CB, Chou YH, Cheng YC, Chang CY, Chiou HJ. Sonographic diagnosis and treatment of a median nerve epineural hematoma caused by brachial artery catheterization. J Ultrasound Med. 2002; 21: 705–708.
- Larsen WJ. Human Embryology. 2nd Ed., Edinburgh, Churchill Livingstone. 1997; 311–339.
- Carlson BM. Human embryology and developmental biology. Philadelphia, Mosby. 2004; 224–225.
- Sannes HD, Reh TA, Harris WA. Development of the nervous system. New York, Academic Press. 2000; 189–197.