Virtual bronchoscopy navigation- An interesting and safe alternative to evaluate deep seated peri-bronchial peripheral lung lesions
Received: 11-Oct-2022, Manuscript No. puljp-22-5463; Editor assigned: 13-Oct-2022, Pre QC No. puljp-22-5463; Accepted Date: Nov 01, 2022; Reviewed: 20-Oct-2022 QC No. puljp-22-5463; Revised: 25-Oct-2022, Manuscript No. puljp-22-5463; Published: 02-Nov-2022
Citation: MK K, Pal V, Utpat K, et al. Virtual bronchoscopy navigationAn interesting and safe alternative to evaluate deep seated peribronchial peripheral lung lesions. J pulmonol. 2022; 6(6):74-77.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Bronchoscopy guided biopsies can help to diagnose pulmonary lesions if endobronchial mass is seen. However a deep seated lung lesions is difficult to get yield if no obvious mass lesions seen during bronchoscopy. A Virtual bronchoscopic navigation (VBN) is a promising navigational bronchoscopy method that guides us to the lung lesions with the virtual images for better yield. The primary purpose of this case report is to present the valuable diagnosing utility of virtual bronchoscopic navigation for deep seated peribronchial peripheral lung lesions
Keywords
Bronchoscopy; Virtual bronchoscopy navigation; Lung cancer
Introduction
Lung cancer is the most common malignancy worldwide after breast cancer. The availability of CT (Computer Tomography) scan screening of the chest has brought an increased number of lung nodules under evaluation. While CT-guided biopsy is one modality to sample lung nodules, it is invasive and has a high rate of complications like pneumothorax, hemorrhage, hem thorax, and ontable death, an alternative method of lung nodule or mass sampling was needed which had more yield and less complication as compared to conventional CT guided biopsy. The high rate of complication of CT-guided biopsy has driven focus to lesser invasive and more targeted modalities like VBN (Virtual Bronchoscopic Navigation). The virtual bronchoscopic navigation method is utilized as a noninvasive guide to navigating the bronchoscope to a peripheral lesion with virtual bronchoscopic images of the bronchial path. This imaging modality uses non-contrast-enhanced computed tomographic images to reconstruct the airways in a three-dimensional manner producing images that appear similar to those visualized during invasive bronchoscopy [1]. While VBN itself cannot acquire samples, it can be used to pre-plan future procedures or as a navigational tool for biopsy. It is a safe effective technique that provides a better diagnostic yield through multiple automated pathways.
Case Report
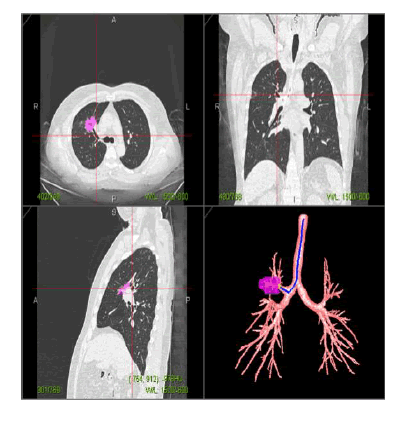
A 66-year-old man presented to our pulmonary medicine department with complaints of dry cough and dyspnea on exertion along with constitutional symptoms including fever, malaise, loss of weight, and decreased appetite for 2 months. The patient had a history of septoplasty 20 years back. No known comorbidities were present. Habitual history and family history were unremarkable. On general examination, his pulse rate, respiratory rate, and blood pressure were 90 beats per minute, 18 cycles per minute, and 110 mmHg/70 mmHg respectively. His transcutaneous oxygen saturation was 97% at room air. Bilateral lower limb swelling was present and dilated veins were seen. His physical examination was otherwise unremarkable. He was evaluated with a plain chest radiograph which was normal hence a high-resolution computer tomography of the thorax was done which revealed a well-defined rounded enhancing hypo dense consolidatory lesion with spiculated margins measuring 3.6 cm*3.2 cm*3 cm in right per hilar region encasing anterior segmental branch of right upper lobar bronchus and right upper lobar pulmonary artery causing mild narrowing of bronchus suggestive of tumor bronchus relationship Type III as per Tsuboi’s classification (Figure 1).
Multiple discrete areas of ground glass opacities in peri-bronchovascular and subpleural regions of bilateral lung parenchyma and a few cm-sized sized enhancing lymph nodes the in the peri-vascular region were present. Full blood counts and biochemistry analysis were within normal limits. Sputum cytology was negative for malignant cells. Further for evaluation of the lesion patient underwent flexible Fiberoptic Bronchoscopy (FBB) with Tran’s bronchial biopsy suggestive of irregular mucosa but no obvious mass lesion was seen at the anterior segment of the right upper lobe bronchus. This was biopsied which was inconclusive. Hence, a Computed Tomography (CT) guided biopsy was planned but was deferred by the radiologist due to the high risk of pneumothorax as a complication in view of the deep-seated lesion. The staging was contemplated to be, stage T2aN0M0 stage IB if NSCLC (Non-Small Cell Lung Carcinoma) and limited disease, resectable disease if SCLC (Small Cell Lung Carcinoma). Therefore to delineate the nature of the lesion and an aggressive approach to rule out lung cancer; a Virtual Bronchoscopic navigation (VBN) was planned as we did not have a radial EBUS (End Bronchial Ultrasound) and C-Arm facility. A VBN protocol CT was done (Figure 2).
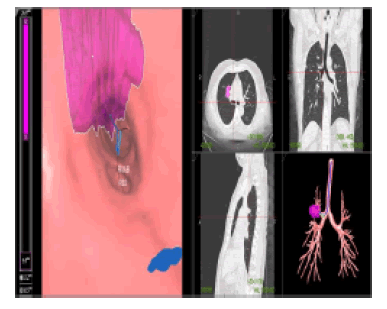
It consisted of a contrast-enhanced computer tomography scan with a slice thickness of less than 1.25 and mm, a slice spacing of less than 0.625 mm. A VBN-assisted trans bronchial biopsy at the anterior segment of the right upper lobe bronchus was attempted (Figure 3).
Histopathological examination of the biopsy revealed non-small cell lung carcinoma favoring adenocarcinoma. Thus VBN was used as a non-invasive image-guided fiducial marker to increase the diagnostic efficacy of the biopsy. The patient was referred to an oncologist where the patient underwent PET–CT (Positron Emission Tomography-CT) which showed a 2.5 cm*2.7 cm*2.7 cm mass in right per hilar region abutting bronchus with multiple ground glass opacities in the right middle lobe. No nodes or distant metastasis were noted. The patient was diagnosed to have adenocarcinoma stage IB so underwent mediastinoscopy followed by right upper bi-lobectomy and pulmonary arthroplasty followed by adjuvant chemoradiotherapy with 3 cycles of cisplatin and pemetrexed and a total of 35 Gy fraction of radiotherapy was given. The patient was doing better till the date of writing the manuscript.
Discussion
Diagnosing deep-seated Peripheral Pulmonary Lesions (PPL) quickly and accurately has always been a clinical difficulty. CT-guided percutaneous lung biopsy has a good diagnostic yield for peripheral lesions but has many complications like pneumothorax, hemorrhage, and others [2]. TBLB (Trans Bronchial Lung Biopsy) has lesser complications but the diagnostic yield of the peripheral lesion is lower. Conventional bronchoscopy can reach up to 4 grade-5 grade bronchus. With the help of ultra-fine bronchoscopy, intratracheal ultrasound, and virtual navigation, the operation field can be extended to 6-grade, 7-grade, or even more distal bronchus, which makes our positioning of pulmonary nodules more accurate. In recent times, VBN has been used along with bronchoscope to diagnose peripheral lung lesions more accurately and with the least complication and without the use of any additional advanced techniques like radial EBUS with C-ARM. Traditional lung biopsy has a yield of 20% and 8% to 20% of lung lesions could not be identified accurately [3]. Virtual navigation technology is one of the new technologies developed in recent years. The image got by high-resolution chest CT without septum scanning is guided into the virtual navigation software system. The three-dimensional reconstruction has the same pixel value range as the inner surface of the bronchus, endows artificial pseudo color and simulates the condition in the lumen, and obtains a dynamic reconstruction image similar to that in the lumen of the bronchus [4]. Navigation bronchoscopy uses a navigational system to guide instruments such as flexible or ultrathin bronchoscopes through the airways to a target lesion for biopsy. Virtual Bronchoscopy Navigation (VBN; also known as Virtual Navigational Bronchoscopy [VNB]) is a technique that utilizes VB Computer Tomographic (CT) imaging to guide the bronchoscope to a peripheral target lesion in the lung [5]. In the first planning phase, the VBN reconstructs the CT data in the DICOM (Digital Imaging and Communications in Medicine) format directly into the navigation software computer, which automatically builds the three-dimensional bronchial tree. CT scan images are acquired with a specialized CT protocol with a slice thickness of < 1.25 mm and slice spacing of < 0.625 mm and transferred to a computer workstation where specific software is used to create a virtual bronchoscopy pathway to the target lesion. It is done usually on the same day or a few days ahead of the planned biopsy procedure. Secondly, the guidance phase during which the acquired virtual images of the airway pathway are displayed and synchronized with real-time images from the bronchoscope (flexible or ultrathin bronchoscope) or until the target lesion is reached. This allows the bronchoscope to be advanced branch-by-branch through the airway to the target lesion [6]. Then a standard brush and biopsy forceps equipment can be placed through the working channel of these scopes to obtain samples from a PPL with or without additional fluoroscopic guidance. VBN has navigation and positioning functions, and the virtual view can be easily advanced and withdrawn according to the requirements. It can directly enter the lesion under its guidance for biopsy. The accuracy of these systems depends upon the quality of the CT data, thus, thin-slice CT scan data and recent CT data from VB-specific protocols are preferred. The precision of VB decreases when CT data are inadequate during VB, and the branching order that can be visualized is lower when slices are too thick [7]. Among the available systems, none incorporate real-time tracking of instruments during the navigation procedure and therefore do not confirm the location of the operating instrument or visualize the target nodule. Thus, VBN increases the chances of biopsying the target PPL (Peripheral Pulmonary Lesion). The overall diagnostic yield by VBN was 80.4% for Peripheral pulmonary lesions. Though VBN was used for peripheral lesions, it can guide to target any lesion for better diagnostic yield like in our case.
Conclusion
VBN is a targeted biopsy modality for lung nodules with minimal complication as compared to CT-guided biopsy especially if deep-seated, peri-bronchial and peripheral. It has a better yield and less complication. The high cost of VBN machines limits its use in low resource setups, but wherever available VBN is currently the best possible approach and should be used instead of conventional CT-guided biopsy which has more complication rate, or blind Trans’ bronchial biopsy which has lesser yields.
References
- Asano F. Virtual bronchoscopic navigation. Clin. chest med..2010 Mar1;31(1):75-85.[GoogleScholar] [CrossRef]
- Rivera MP, Mehta AC, Wahidi MM. Establishing the diagnosis of lung cancer: Diagnosis and management of lung cancer: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013 May 1;143(5):e142S-65S.[GoogleScholar] [CrossRef]
- Xu C, Yuan Q, Chi C, et al. Computed tomography-guided percutaneous transthoracic needle biopsy for solitary pulmonary nodules in diameter less than 20 mm. Medicine. 2018 Apr;97(14).[GoogleScholar] [CrossRef]
- Asano F, Eberhardt R, Herth FJ. Virtual bronchoscopic navigation for peripheral pulmonary lesions. Respiration. 2014;88(5):430-40. [GoogleScholar] [CrossRef]
- Levine MZ, Goodman S, Lentz RJ, et al. Advanced Bronchoscopic Technologies for Biopsy of the Pulmonary Nodule: A 2021 Review. Diagnostics. 2021 Dec 8;11(12):2304. [GoogleScholar] [CrossRef]
- Liu Y, Wang F, Zhang QC, et al. Value of virtual bronchoscopic navigation and transbronchial ultrasound-guided sheath-guided exploration in the diagnosis of peripheral lung cancer. World J. Clin. Cases. 2020 Aug 8;8(16):3450.[GoogleScholar] [CrossRef]
- Ishida T, Asano F, Yamazaki K, et al. Virtual Navigation in Japan (V-NINJA) Trial Group. Virtual bronchoscopic navigation combined with endobronchial ultrasound to diagnose small peripheral pulmonary lesions: a randomised trial. Thorax. 2011 Dec 1;66(12):1072-7. 1;66(12):1072-7. .[GoogleScholar] [CrossRef]