A Rare Case of Brachial Artery Aneurysm in a Young Adult Clinical Presentation, Diagnosis, and Management
Received: 04-Jul-2023, Manuscript No. ijav-23-6616; Editor assigned: 05-Jul-2023, Pre QC No. ijav-23-6616 (PQ); Accepted Date: Jul 24, 2023; Reviewed: 19-Jul-2023 QC No. ijav-23-6616; Revised: 24-Jul-2023, Manuscript No. ijav-23-6616 (R); Published: 31-Jul-2023, DOI: 10.37532/1308-4038.16(7).289
Citation: Karl M. A Rare Case of Brachial Artery Aneurysm in a Young Adult Clinical Presentation, Diagnosis, and Management. Int J Anat Var. 2023;16(7):353-354.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Brachial artery aneurysms are uncommon vascular pathologies, especially in young adults. We present a case of a 27-year-old male who presented with an enlarging pulsatile mass in the right arm. Imaging studies revealed a brachial artery aneurysm, and the patient underwent successful surgical intervention. This case report discusses the clinical presentation, diagnostic approach, and management strategies employed in this rare vascular anomaly.
Keywords
Brachial artery, Aneurysm, Young adult, Diagnosis, Surgical intervention
INTRODUCTION
Brachial artery aneurysms are uncommon vascular abnormalities characterized by localized dilations in the brachial artery. While typically associated with atherosclerosis and seen in elderly patients, they rarely occur in young adults. This case report presents a unique instance of a brachial artery aneurysm in a 27-year-old male, highlighting the importance of recognizing and managing this rare vascular anomaly [1].
The etiology of brachial artery aneurysms in young adults remains unclear, making their diagnosis and treatment challenging. Non-invasive imaging modalities, such as color Doppler ultrasonography and computed tomography angiography (CTA), play a pivotal role in accurate diagnosis and surgical planning [2]. Surgical repair is often the preferred treatment to avoid potential complications, with the choice of approach depending on individual patient factors. This case report emphasizes the significance of a multidisciplinary approach involving vascular surgeons, radiologists, and anesthesiologists in managing this condition successfully [3].
Given the scarcity of reported cases in young adults, documenting and sharing the clinical course and treatment outcomes are vital to expand medical knowledge and improve awareness among healthcare professionals. An improved understanding of brachial artery aneurysms will enable more effective and individualized care for affected patients [4-5].
CASE REPORT
A 27-year-old male presented to our vascular clinic with a four-month history of a gradually enlarging pulsatile mass in his right upper arm. The patient reported mild intermittent discomfort in the region, but no significant pain, numbness, or weakness. There was no history of trauma or known connective tissue disorders. Family history was unremarkable for vascular diseases. Physical examination revealed a 4-cm palpable, pulsatile mass in the right brachial region, with no distal ischemic changes.
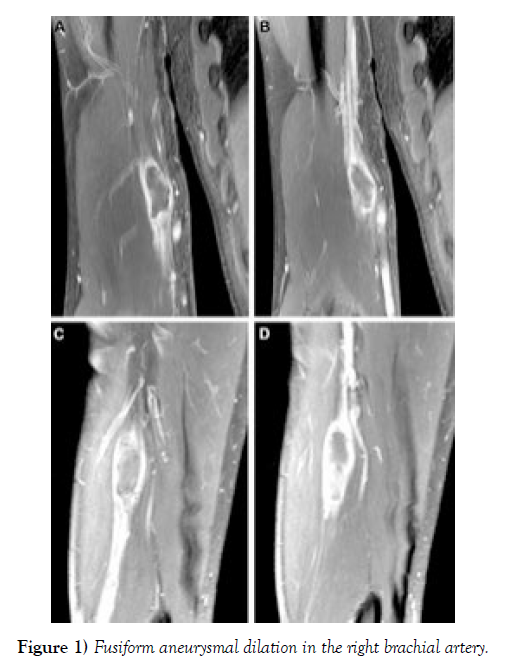
Diagnostic Workup: Color Doppler ultrasonography was performed, revealing a fusiform aneurysmal dilation in the right brachial artery, measuring approximately 3.8 cm in diameter. The surrounding soft tissues appeared normal, and there were no signs of thrombosis. To further characterize the aneurysm, computed tomography angiography (CTA) was conducted, confirming the presence of a saccular aneurysm arising from the brachial artery. The aneurysm measured 4.2 cm in its widest diameter (Figure 1). Additionally, the patient underwent blood tests, which revealed normal lipid profiles and inflammatory markers, ruling out atherosclerosis or vasculitis as the underlying cause.
Diagnosis: Based on the imaging findings and clinical presentation, the patient was diagnosed with a brachial artery aneurysm. Considering the rarity of this condition in young adults and the potential risk of complications, a multidisciplinary team, including vascular surgeons, radiologists, and anesthesiologists, convened to discuss the optimal management approach.
Management: Given the size of the aneurysm and the potential for complications such as thrombosis, embolization, or rupture, surgical intervention was recommended. The patient was thoroughly counseled about the procedure, its risks, benefits, and alternative treatments. Informed consent was obtained.
Under general anesthesia, the patient underwent an open surgical repair of the brachial artery aneurysm. A longitudinal incision was made over the right brachial artery, and the aneurysm was carefully exposed. After systemic heparinization, clamps were applied proximally and distally to the aneurysm, and the aneurysm sac was opened. Thrombectomy was performed to clear any intraluminal thrombus. Subsequently, the aneurysm was resected, and end-toend anastomosis was performed using a polytetrafluoroethylene (PTFE) graft. Hemostasis was achieved, and the wound was closed in layers [6].
Postoperative Course: The patient’s postoperative recovery was uneventful, with no immediate complications noted. He was discharged on postoperative day four with instructions for arm immobilization and a course of oral anticoagulation to prevent thrombosis within the graft [7].
Follow-up: Follow-up appointments were scheduled at regular intervals, and duplex ultrasound scans were performed to monitor the patency of the graft and the absence of any recurrent aneurysmal dilation. Six months postsurgery, the patient showed satisfactory progress, with no evidence of graft stenosis, occlusion, or aneurysm recurrence.
DISCUSSION
Brachial artery aneurysms are a rare entity, and their occurrence in young adults is even rarer. The etiology of isolated brachial artery aneurysms remains largely idiopathic, but certain predisposing factors, such as trauma, connective tissue disorders, or infections, may contribute to their development. In the absence of these factors in our patient, the aneurysm was likely congenital or degenerative in nature.
Diagnosing brachial artery aneurysms relies heavily on non-invasive imaging modalities such as Doppler ultrasonography and CTA. While ultrasonography provides real-time vascular mapping, CTA offers detailed three-dimensional visualization, aiding in surgical planning.
Surgical intervention is often the preferred treatment for brachial artery aneurysms, as conservative management carries a risk of complications. Open surgical repair with end-to-end anastomosis using synthetic grafts has been the standard approach. However, endovascular techniques, such as stent-graft placement, have also been employed successfully in certain cases, particularly in older patients with complex medical histories [8-10].
CONCLUSION
Brachial artery aneurysms in young adults are uncommon vascular pathologies. This case report highlighted the importance of early diagnosis and appropriate management to prevent severe complications.
Non-invasive imaging techniques, such as Doppler ultrasonography and computed tomography angiography, play a crucial role in accurate diagnosis. Surgical intervention remains the preferred treatment, providing excellent long-term outcomes and reducing the risk of life-threatening complications. A collaborative, multidisciplinary approach involving vascular surgeons, interventional radiologists, and anesthesiologists is essential in managing these cases.
Further research is needed to better understand the etiology and risk factors associated with brachial artery aneurysms in young adults. Regular follow-up and monitoring post-surgery are crucial to detect any anomalies promptly.
Raising awareness about this condition among healthcare professionals is important for early identification and timely intervention. In conclusion, early diagnosis, multidisciplinary care, and continuous follow-up are crucial in managing brachial artery aneurysms in young adults. Further research can enhance our understanding and improve treatment strategies for this rare vascular anomaly.
ACKNOWLEDGEMENT
The authors would like to acknowledge the patient for granting permission to present his case, as well as the medical and nursing staff involved in his care.
CONFLICT OF INTEREST
The author declares no conflicts of interest related to this case report.
REFERENCES
- Kovac JD, Stankovic A, Stankovic D, Kovac B, Saranovic D, et al. Intracranial arterial variations: A comprehensive evaluation using CT angiography. Med Sci Monit. 2014; 20:420-427.
- Van Vuuren AJ, Saling MM, Ameen O, Naidoo N, Solms M, et al. Hand preference is selectively related to common and internal carotid arterial asymmetry. Laterality. 2017; 22(4):377-398.
- Hakim A, Gralla J, Rozeik C, Morddasini P, Leidolt L, et al. Anomalies and normal variants of the cerebral arterial supply: A comprehensive pictorial review with a proposed workflow for classification and significance. J. Neuroimaging. 2018; 28: 14-35.
- Sun Y, Shi Y-M, Xu P. The clinical research progress of vertebral artery dominance and posterior circulation ischemic stroke. Cardiovasc Dis. 2022; 51:553-556.
- Vural A, Cicek ED. Is asymmetry between vertebral arteries related to cerebral dominance? Turk J Med Sci. 2019; 49: 1721-1726.
- Gaigalaite V, Dementaviciene J, Vilimas A, Kalibatiene D. Association between the posterior part of the circle of Willis and vertebral artery hypoplasia. PLoS ONE. 2019; 14(9): e0213-226.
- Mujagic S, Kozic D, Huseinagic H, Smajlovic D. Symmetry, asymmetry and hypoplasia of intracranial internal carotid artery on magnetic resonance angiography. Acta Med Acad. 2016; 45:1- 9.
- Rusu MC, Vrapclu AD, Lazar M. A rare variant of accessory cerebral artery. Surg Radiol Anat. 2023; 45(5):523-526.
- Mani K. Absent internal carotid artery in the circle of Willis. IOSR-JDMS. 2015; 14(11): 38-40.
- Dumitrescu Am, Cobzaru RG, Ripa C, TanaseMD, Sorodoc V, et al. Anatomical variation of the anterior part of the circle of Willis- an Autopsic study. J Univers Surg. 2021; 9(4): 21.
- Wu T-C, Chen T-Y, Ko C-C, Chen J-H, Lin C-P, et al. Correlation of internal carotid artery diameter and coronary flow with asymmetry of the circle of Willis. BMC Neurology. 2020; 20:251.
- Barbato F, Allocca R, Bosso G, Numis FG. Anatomy of cerebral arteries with clinical aspects in patients with ischemic stroke. Anatomia. 2022; 1:152-169.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref