Role of CRTH2 in Eosinophil Infiltration of Recurrent Nasal Polyps
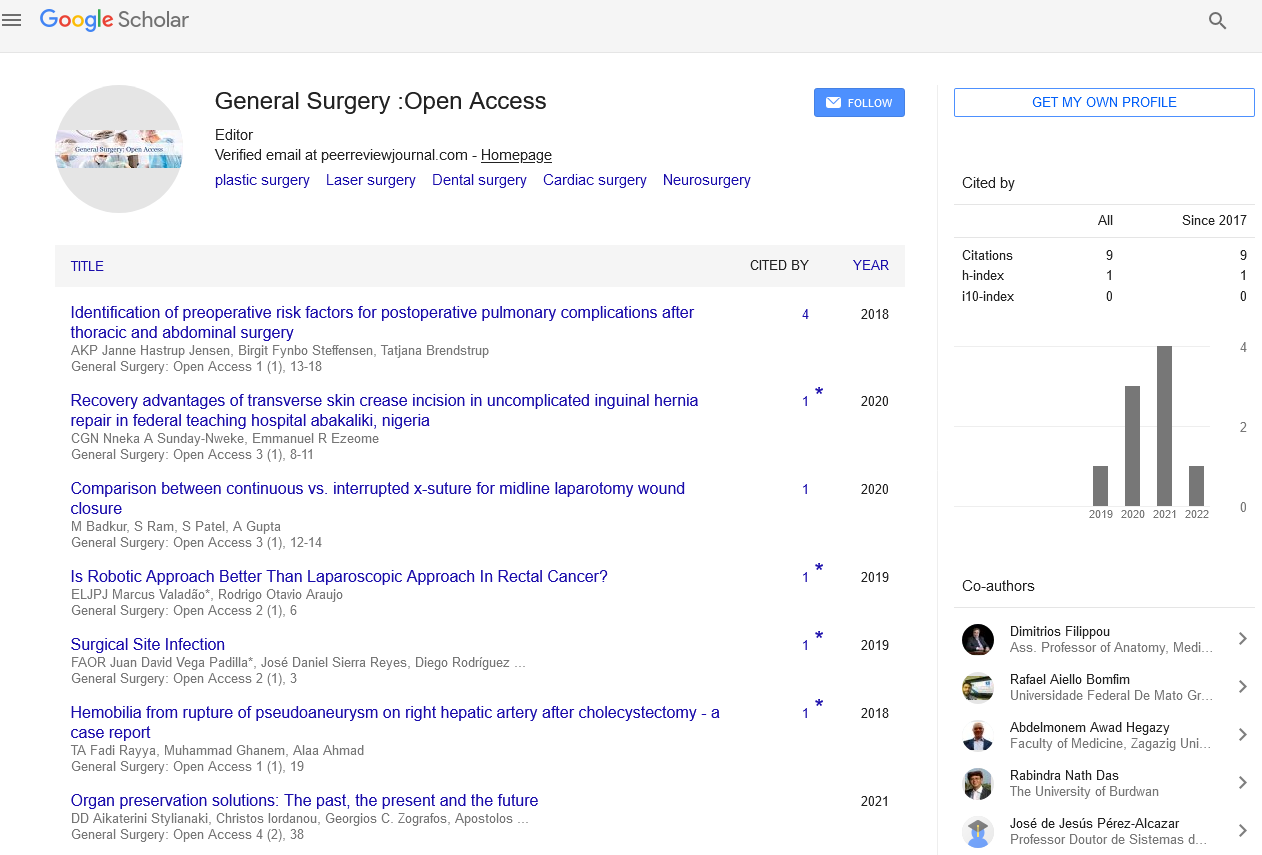
Received: 03-Dec-2021, Manuscript No. PULGSOA-22; Editor assigned: 08-Jan-2022, Pre QC No. PULGSOA-22(PQ); Accepted Date: Jan 05, 2022; Reviewed: 18-Dec-2021 QC No. PULGSOA-22(QC); Revised: 04-Jan-2022, Manuscript No. PULGSOA-22(R); Published: 14-Jan-2022, DOI: 10.37532/pulgsoa.2022.5(1)-01
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Chronic rhinosinusitis with nasal polyps (CRSwNP) is a difficult-to-treat disease that is often characterized by recurrent nasal polyp (NP) growth even following surgical removal, but the mechanisms that underlie the pathogenesis of polyp recurrence are still not clear.
Objectives: This study aimed to investigate the expression of chemoattractant receptor-homologous molecule expressed on Th2 cells (CRTH2) receptor on eosinophils of patients with nasal polyps and the role it plays in eosinophil infiltration and nasal polyp recurrent.
Methods: mRNA was extracted from recurrent nasal polyp, nasal polyps, control group and evaluated for expression of CRTH2. Immunofluorescence staining was performed to confirm theexpression of CRTH2 protein. CRTH2 expression on peripheral blood eosinophils was quantified by flow cytometry as being side scatterhigh, CD16-, Siglec8+ and CRTH2+.
Results: : Gene expression analysis revealed that nasal polyps display increased level of CRTH2 compared with control samples, with the highest expression showed in the recurrent nasal polyps. Immunofluorescence confirmed the higher expression of CRTH2 on eosinophils of recurrent nasal polys, which correlated with the number of tissue eosinophils. Peripheral blood eosinophils from recurrent nasal polyps displayed higher expression of CRTH2 which is confirmed by flow cytometry.
Conclusion: The PGD2-CRTH2 pathway may play an important role in eosinophil infiltration in nasal polyps, which may play an important role in nasal polyp recurrence. These results open channels for therapeutic modalities targeting CRTH2 molecules in recurrent nasal polyps.include a surgeon experienced in vascular surgery and an anaesthesiologist.
Introduction
Eosinophils are a unique lineage of granulocytic leukocytes that have been detected in the blood and specific tissues for over a century. Since their discovery in practically all vertebrates, not just humans, these unique cells with their particular panoply of proteins, organelles, and other properties have been implicated in a wide range of pathophysiologic and beneficial responses to their hosts. Eosinophils' homeostatic contributions span from participation in innate immune responses to parasite invaders like helminths to contributions to tissue regeneration, fat metabolism, and other responses.
Eosinophils will be problematic: a rise in their range and activation has been coupled to a spread of diseases, as well as respiratory illness, eczema, leukocyte channel disorders, hypereosinophilic syndromes, and more, additionally because of the focus of this review, chronic rhinosinusitis (CRS) with or while not nasal polyps (CRSwNP and CRSsNP, respectively). for instance, in patients with Samter's triad, currently referred to as an aspirin-exacerbated disease, "cells found in nasal polyps aren't restricted to any specific sort, though lymphocytes area unit rare and eosinophils tend to occur in conspicuous numbers," and at the time, the leading theory was that eosinophils were "...indicators of antigen-antibody reactions of the immediate, histamine-releasing, nasal polyps.
In 2020, despite enormous gains in knowledge and the availability of medications that target type 2 inflammation and even eosinophils themselves, our understanding of CRS pathophysiology with or without nasal polyposis, particularly the involvement of eosinophils in these illnesses, remains unsatisfactory. Following is an introduction of eosinophil biology in terms of its possible contributions to CRS pathophysiology, followed by a synopsis of what is known about eosinophils and their mediators in samples collected from patients with CRSwNP and CRSsNP. The review finishes with a discussion of the lessons learned as a consequence of novel pharmacology capable of targeting type 2 inflammation and eosinophils in various disorders, as well as instances of outstanding questions and prospects.
Several plausible paths emerge when evaluating processes of local eosinophil recruitment, retention, survival, and activation. Cell surface adhesion molecules such as P-selectin, beta 1 integrins such as VLA-4, and beta 2 integrins are almost certainly involved in their preferential recruitment, interacting with their respective counterligands expressed on inflamed endothelial sinus mucosa (P-selectin ligand [CD162], VCAM-1, and ICAM-1, among others). When compared to most other circulating cells, a distinct group of chemotactic factor receptors, such as CCR3, CRTh2, and CysLT1, allow eosinophils to migrate preferentially and directionally into the extravascular compartment. ewer pharmacology capable of targeting type 2 inflammation and eosinophils in various disorders, concluding with instances of outstanding questions and proposals for future studies.
Aside from their selective accumulation, eosinophils show indications of longer survival in nasal tissue, which is likely owing to protection from cell death by locally generated cytokines such as interleukin (IL)- 5 and granulocyte-macrophage colony-stimulating factor. Beyond their accumulation and extended survival inside the nasal mucosa, what eosinophils create and release as part of their contribution to the inflammatory response may be more crucial. Even though the processes of eosinophil activation are yet unknown, it is known that eosinophils release a diverse spectrum of chemicals.
Some are prefabricated and kept in the form of granules. Indeed, evidence of commitment to the creation of eosinophil granule proteins is particularly prevalent throughout the eosinophil genome. The crystalloid core of particular granules includes the main basic protein, whereas the granule matrix stores eosinophil cationic protein (ECP), eosinophil-derived neurotoxin (EDN), eosinophil peroxidase (EPX), secretory phospholipase A2, and other proteins.
Galectin-10, enzymes, cytokines, growth factors, and chemokines are among the other proteins generated by human eosinophils. Many of these eosinophil granule proteins may be found in nasal biospecimens, while other proteins, such as galectin-10 (previously known as Charcot-Leyden crystal [CLC] protein, which accounts for up to 10% of total protein in eosinophils), have been demonstrated to cause inflammation.