Page 20
Volume 03
Spine 2019
October 16-17, 2019
Journal of Neurology and Clinical Neuroscience
October 16-17, 2019 | Rome, Italy
SPINE AND SPINAL DISORDERS
5
th
World Congress on
J Neurol Clin Neurosci, Volume 03
Treatment of Toracolumbar Transition Fractures type A3 and A4: Prospective study
of pain and quality of life in Open vs. Percutaneous Arthrodesis
Gibran Franzoni Rufca
1
, Carla de Jiacomo Machado Gazola
1
, Mario Wolak Junior
2
, Leon Cleres Pinheiro
2
,
Flávio Ramalho Romero
2
, Flávio Porto Franco Piola
3
, Georgea Carneiro
3
and
Ana Carolina Fonseca Galoti
4
1
Hospital Santa Casa de Ourinhos, Brazil,
2
Universidade Estadual Paulista – UNESP, Brazil
3
Hospital Regional Presidente Prudente, Brazil,
4
Hospital Regional de Assis, Brazil
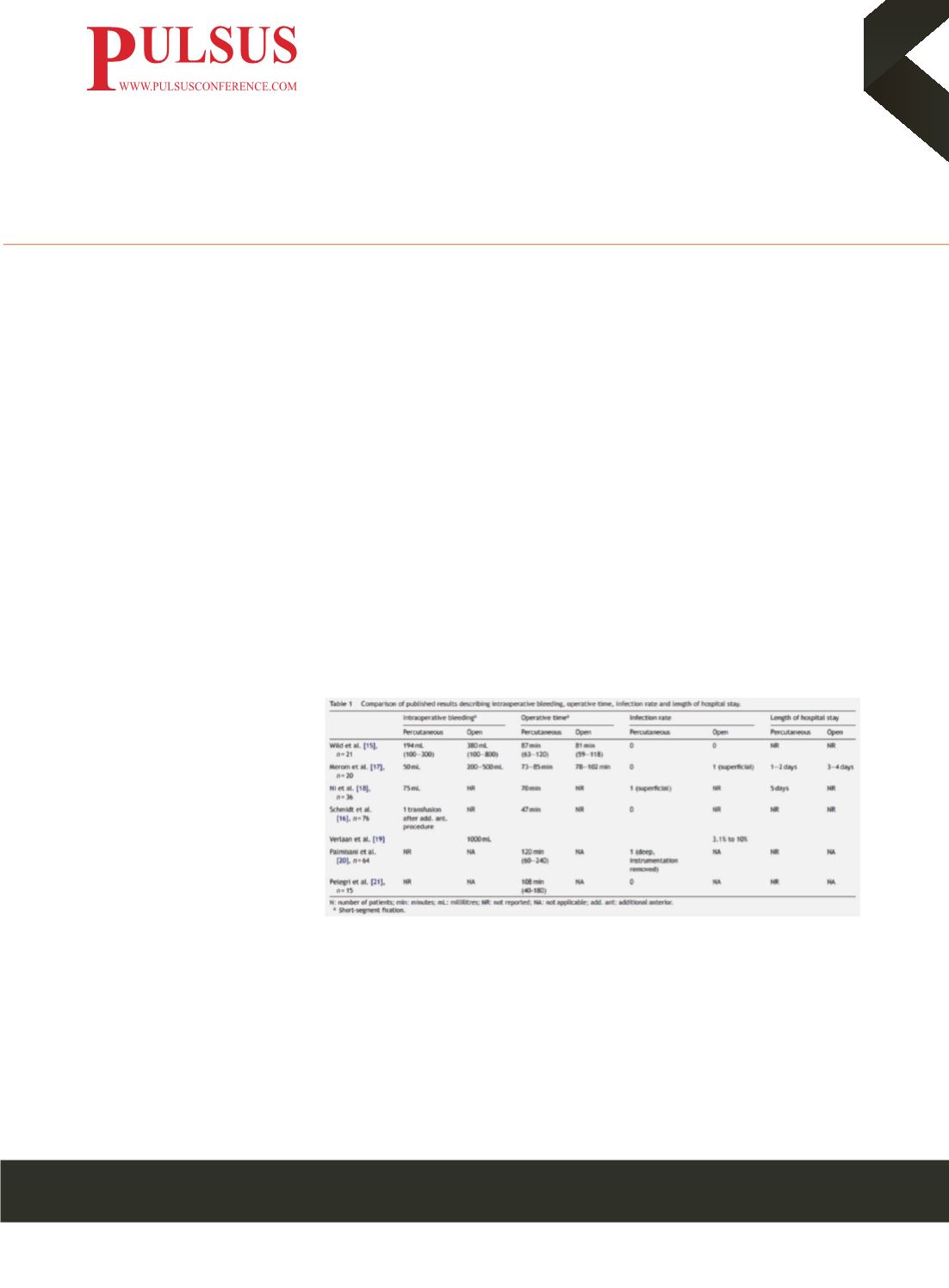
A
pproximately 11,000 new cases of Spinal Injuries occur every year in the United States and approximately 250,000 people
in this country have associated Spinal Cord Injury. The life expectancy for patients is shortened from 15 to 20 years. In the
treatment, the open posterior approach, with midline incision for decompression and fusion is one of the most used techniques.
However, is associated with the aggression of healthy tissue, muscle injury and increased rate of bleeding. In this context, Minimally
Invasive Techniques have been increasingly used, with less damage to healthy tissues, less bleeding and reduced morbidities and
complications. Nowadays, data favoring one technique over the other are insufficient, with a low number of patients studied,
leading to inconclusive results and low clinical impact. Therefore, a prospective, longitudinal, multicenter study is being developed
with the follow-up of individuals for 12 months. The primary objective is of assessing whether, for the treatment of Thoracolumbar
Fractures, Minimally Invasive Surgery is superior to conventional surgery regarding postoperative pain and Quality of Life (QoL).
All patients are being submitted to preoperative X-ray and computed tomography of the spine for decision-making and calculation
of deformities. After the patients' written consent, an instrument containing the following data is being applied: demographic,
hospitalization, clinical and neurological conditions and biomechanics. The following intraoperative data are being analyzed:
type of surgery, number of levels fused, number of screws used, need for Laminectomy, need for previous instrumentation, blood
loss, surgical time and occurrence
of complications. The prognostic
analysis is being performed through
the application of pain and (QoL)
questionnaires: Visual Analog Pain
Scale, Oswestry Disability Index and
SF-36. These assessments are being
done at 15 days, 03, 06, 12 months
after surgery. In this presentation,
we will present the partial results
obtained so far and the comparison of
these with current literature.
Biography
Gibran Franzoni Rufca has completed his degree in Medicine and Neurosurgery from the School of Medicine of São José do Rio Preto.
He lives in the state of São Paulo and his main institution is the Hospital Santa Casa de Ourinhos, where he and his team provide
Neurosurgical Treatments, mainly for the pathologies of the Vertebral Column.
Gibran Franzoni Rufca and his team who were brought the first endoscopic functional surgeries and minimally invasive procedures of
the spine into their region. In constant updating, inside and outside the country, He is currently also a master's degree student in the
Post-Graduation Program of the University of São Paulo - Campus Botucatu where he is working in the research of Pain and Minimally
Invasive Surgeries of the spine, under the coordination of Prof. Dr. Flávio Ramalho Romero.
e
:
gibran.rufca@gmail.comFigure 1 C. Court, C. Vincent. Orthopaedics & Traumatology: Surgery & Research (2012) 98, 900—909
















